Contents
Stomach ulcer and duodenal ulcer (peptic ulcer)
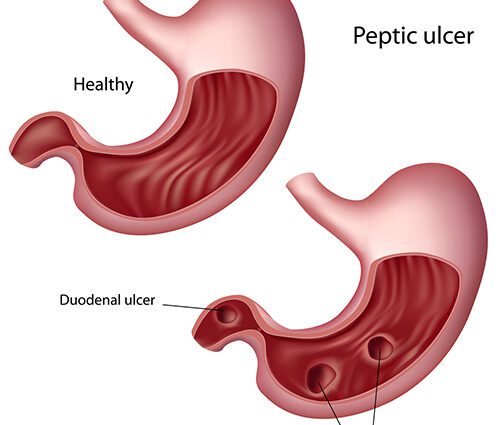
L’peptic ulcer, also called a gastric ulcer if it is located in the stomach and called duodenal ulcer when it forms in the duodenum (the first part of the small intestine), are somehow wounds form of erosion that penetrates deep into the wall of the digestive tract (see diagram).
These wounds are often painful: they enter directly in touch with theacid present in the digestive tract. A situation comparable to applying an alcohol swab on a scratch.
The expression ” peptic ulcer »Includes, because of the similarity of their manifestations, gastric ulcer and duodenal ulcer
It is estimated that about 10% of the population of industrialized countries is likely to suffer from an ulcer at one time or another. The elderly of 40 and over are the most affected. Duodenal ulcers are 10 times more common than stomach ulcers.
Causes
La bacterium Helicobacter pylori (H. Pylori), a bacterium that survives acidity, is the main cause of ulcers: it is thought to cause approximately 60% to 80% of stomach ulcers and 80% to 85% of duodenal ulcers. These bacteria invade the mucus layer that normally protects the stomach and small intestine from acidity, and are believed to disrupt this protective mechanism in some people. In industrialized countries, 20% of people aged 40 and under have this bacteria in their digestive tract. A proportion that reaches 50% among those over 60. About 20% of carriers of the bacteria will develop an ulcer during their lifetime.
Takinganti-inflammatory Nonsteroidal drugs or NSAIDs (for example, Aspirin, Advil® and Motrin®), is the second most common cause of ulcer in the digestive tract. The combination of infection with the bacteria H. Pylori and taking anti-inflammatory drugs synergistically increases the risk of ulcers. The risk is then 60 times greater.
Here are other causes:
- A excessive acid production through the stomach (gastric hyperacidity), attributable to smoking, excessive alcohol consumption, severe stress, hereditary predisposition, etc. However, these could be aggravating factors rather than the true causes of ulcers.
- A severe burn, injury important or even the physical stress associated with serious illness. This creates “stress ulcers”, which are often multiple and are most often located in the stomach, sometimes at the very beginning of the small intestine (in the proximal duodenum).
- More rarely, a stomach ulcer may turn out to be stomach cancer that has ulcerated.
Acids and antacids in the digestive tract In the wall of thestomach, glands secrete gastric juices which contribute to the digestion :
The contents of the stomach are still acid. Its pH varies from 1,5 to 5, depending on the food ingested and also depending on the individual. Other glands secrete mucus intended for protect the inner walls of the stomach:
The wall of thesmall intestine is also covered with a mucus layer which protects it from the acidity of the chyme, name given to the “food porridge” which comes from the stomach. |
Evolution
Usually an ulcer appears gradually in a few weeks. It can also appear quickly, after a few days of taking nonsteroidal anti-inflammatory drugs, for example, but this situation is not very common.
The rate of healing spontaneous could be around 40% (over a 1 month period), especially if the ulcer was caused by taking NSAIDs and they are stopped. Spontaneous definitive healing, without relapse, is however rare. Smokers are more likely to relapse than non-smokers.
If the ulcer is not treated or the cause is not corrected, there is a strong possibility that the ulcers will reappear within a year. But even with good treatment, there is a recurrence in 20-30% of cases.
Possible complications
Complications are relatively rare. THE’ulcer can cause a hemorrhage : blood then flows inside the digestive tract. The bleeding is sometimes massive, with vomiting of red or coffee-bean-like blood, with blood in the stool that may be red or black. The bleeding can also be quiet and relatively slow. You may or may not notice that the stool turns black. Indeed, under the influence of digestive juices, the blood turns black. Bleeding can cause anemia over time if it goes undetected. The first symptom of the ulcer may be bleeding, without pain previously, especially in older people. You must consult a doctor without delay.
Another complication, much less common than bleeding, is perforation complete wall of the digestive tract. This situation causes violent abdominal pain, which quickly worsens in peritonitis. This is a medical and surgical emergency.