Peristalsis: what to do in case of intestinal peristalsis?
Intestinal transit is easily disturbed. Although not serious in the vast majority of cases, it happens that the muscular contractions which ensure the progression of food in the digestive tract, intestinal peristalsis, are too weak or on the contrary too fast. These inconveniences can be annoying on a daily basis. Update on its operation?
Anatomy of intestinal peristalsis?
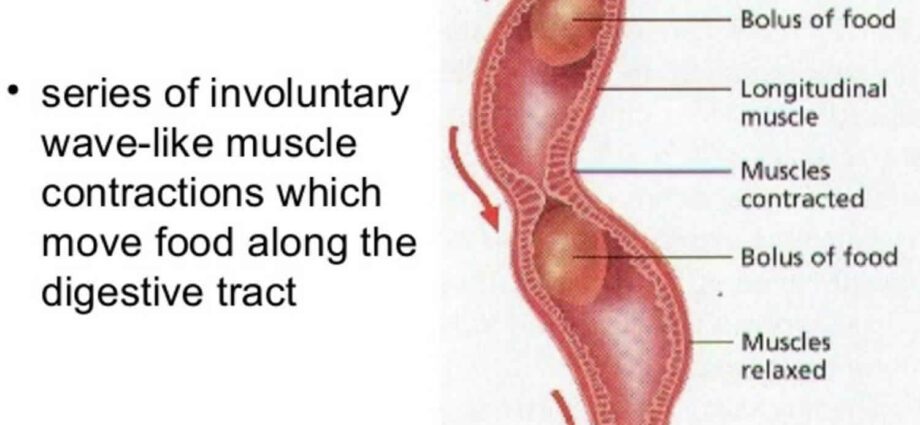
We call “peristalsis” all the muscular contractions (“peristaltic movements”) of the digestive tract which are done from top to bottom allowing the progression of food inside a hollow organ. In other words, the walls of the esophagus propel food to the stomach through rhythmic movements produced by muscle contractions.
The word derives from neo-Latin and comes from the Greek peristallein, “to surround”.
Thanks to the muscles which surround them, the hollow organs, esophagus, stomach and intestine, contract spontaneously, allowing the progressive advance of food. Without this phenomenon, all the processing of food and absorption of nutrients would be impossible.
Digestive laziness and impaired intestinal peristalsis often cause chronic complications.
What are the causes of a slowdown in intestinal peristalsis?
The motor skills of the smooth muscles of the digestive tract and the intestinal peristalsis can be degraded by multiple factors.
The reasons for this peristaltic slowdown can be of origin:
- Hormonal: pregnancy, menopause, taking a hormonal contraceptive;
- Organic: pathology or old age;
- Iatrogenic: repeated medication;
- Psychogenic or social: anorexia nervosa, depression;
- Healthy lifestyle: sedentary lifestyle: associated with a reduction in peristaltic movements: the digestive tract becomes in all senses of the term “lazy”, poor diet: mainly the lack of fiber in the diet, lack of hydration: a decrease in water intake in general, stress or change in habits (change of life, travel or anxiety can seriously disrupt peristalsis).
What are the pathologies linked to intestinal peristalsis?
Digestive laziness and impaired intestinal peristalsis often cause chronic complications such as:
- Functional colopathy or irritable bowel syndrome: functional pathology, that is to say that the functioning of the intestine is altered and reacts too actively causing episodes of diarrhea or constipation;
- Fecaloma: a disorder of the digestive tract characterized by an abnormal accumulation of feces. It is one of the complications of chronic constipation;
- Gastroparesis: manifested by delayed gastric emptying, the stomach empties poorly or too slowly;
- Achalasia: pathology in which the muscles of the esophageal wall as well as the sphincter located between the esophagus and the stomach do not relax after swallowing, which prevents food from entering the stomach;
- Intestinal ileus: temporary stoppage of intestinal peristalsis which most often appears after abdominal surgery, particularly when the intestines have been manipulated;
- Occlusive Syndrome: Bowel obstruction manifests as abdominal pain, stopping of materials and gas, nausea or vomiting, abdominal meteorism and often requires emergency surgery while others allow medical treatment.
What treatment for intestinal peristalsis?
Treatments for intestinal peristalsis are linked to treatments for diarrhea (watery stools more than three times a day or more often than usual) or constipation.
In case of diarrhea
- Take care to prevent possible dehydration: the water does not contain enough mineral salts, it is better to drink degassed cola, rich in electrolytes;
- Favor a diet that invigorates: rice, cooked carrots, fruit compotes, bananas, or quince jelly, and reduce raw fruits and vegetables which increase bowel movements;
- Rescue drugs: Smecta or other analogues active on heartburn and diarrhea.
In case of constipation
- Eat healthy: cut down on fats, excess alcohol and processed foods;
- Favor products rich in fiber (green vegetables, dried fruits, whole grain bread cereals);
- Take the time to eat;
- Stay hydrated by drinking water;
- Practice regular physical activity (swimming, jumping and running sports, brisk walking, etc.).
Ileus
Treatment includes:
- Aspiration nasogastrique ;
- A fasting;
- An IV hydroelectrolytic supply: to compensate for losses prior to the operative act but also to take into account the effects due to the act and the anesthesia technique. In the event of an occlusive syndrome related to peristalsis paralysis, it is the treatment of the cause that is important.
What diagnosis in case of intestinal peristalsis?
No biological examination is essential for the diagnosis. The recommendation proposes a blood test with the search for anemia or a CRP test in order to look for inflammation, and finally to carry out a possible screening for celiac disease.
The warning signs leading to promptly performing a colonoscopy are:
- des rectorragies;
- unexplained weight loss
- a family history of colon cancer;
- discovery of clinical abnormality (abdominal mass);
- the onset of the first symptoms after 60 years.