Contents
In line with its mission, the Editorial Board of MedTvoiLokony makes every effort to provide reliable medical content supported by the latest scientific knowledge. The additional flag “Checked Content” indicates that the article has been reviewed by or written directly by a physician. This two-step verification: a medical journalist and a doctor allows us to provide the highest quality content in line with current medical knowledge.
Our commitment in this area has been appreciated, among others, by by the Association of Journalists for Health, which awarded the Editorial Board of MedTvoiLokony with the honorary title of the Great Educator.
Influenza is a serious viral respiratory infection with the highest death rate. Influenza epidemiology covers seasonality (winter months of the year), worldwide prevalence and virus type. Changes in the antigens of the individual strains of the virus are observed every year. The incidence of influenza gives only short-term immunity – up to several months, and only against the type of virus that caused the disease. Influenza is caused by influenza A and B viruses. Infection occurs through airborne droplets or direct contact.
A few words about the flu
Influenza is a group of clinical symptoms associated with an acute respiratory infection. The disease is caused by viruses from the Orthomyxoviridae family. In turn, viruses are divided into three types: type A, type B and type C1. Type A is divided into subtypes according to the nature of the two proteins on the surface of the molecule: haemagglutinin (H) and neuraminidase (N). According to the World Health Organization, up to 10% of people suffer from flu every year. adults and 30 percent. kids. The need for hospitalization occurs in the elderly and chronically ill.
Seasonal flu – occurs every year during the epidemic period and is caused by human influenza viruses: the most common are viruses of the H1N1 and H3N2 subtypes.
Pandemic flu – it is characterized by the occurrence of a global epidemic every several or several dozen years. Pandemic flu is caused by different types of viruses. The infection spreads very quickly as most people do not have immunity to the new types of virus. Thus, the number of people suffering from influenza in the endemic period is much greater than in the case of seasonal influenza. The WHO usually reports the occurrence of a pandemic on the basis of information on the geographical spread of infections with a new type of virus.
The duration, severity, onset, and peak of flu season may vary from year to year. This is due to many factors, such as the fact how much the virus differs from those that circulated in previous seasons. Sometimes the number of cases in a given area is much greater than usual. Then it is often referred to as an epidemic. City / country authorities may declare a pandemic, which at the same time entails the use of various methods of prevention by sanitary and epidemiological services. Schools and workplaces are often closed. In addition, decisions are made to close borders and people are obligated to compulsory vaccination against influenza.
Influenza epidemiology
Although flu is common, it is much rarer than the common cold. Up to several million Poles suffer from the flu every year. Considering the fact that colds are caused by various types of viruses, infection can occur even several times a year.
As an aid to treating flu symptoms, try Rosehip or Linden Flower, which can be purchased as a herbal tea.
The causes of the flu
Type A and B viruses are the etiological factor of pandemic influenza. The former is further divided into subtypes, based on the antigen specificity of two surface proteins: haemagglutinin (H) and neuraminidase (N). In turn, seasonal flu is caused by viruses: H1N1 and H3N2, sometimes it is the H1N2 virus. Seasonal flu usually falls from fall to early spring (northern hemisphere), while in the southern hemisphere it is from spring to late summer. Recently, people (mainly from Asia and Egypt) have been diagnosed with diseases caused by the avian influenza virus (H5N1), which is associated with a high percentage of mortality. In 2009, an epidemic with the A / H1N1 virus, known as the so-called swine flu (although the term is incorrect as the virus is a reassortant derived from human, swine and avian influenza virus strains).
Prophylactically, as a strengthening of immunity, drink the juices from the Healthy as Fish set – a set of fruit and vegetable shots with herbs, which consist of apple juice, lemon juice, ginger juice, parsley juice.
The mechanism of influenza formation
The influenza virus multiplies in epithelial cells of the upper and lower respiratory tract. The symptoms occurring in the course of the disease are a consequence of the influence of cytokines, which are released in the course of an inflammatory reaction. Comparing typical seasonal influenza viruses: the A / H1N1v virus has a greater affinity for the epithelial cells of the lower respiratory tract. Moreover, it penetrates deeper into the respiratory system.
The reservoir of the influenza virus is humans and certain animals (e.g., pet birds or pigs). Influenza infection is usually transmitted by airborne droplets, although there are cases of infection through contact with contaminated objects or through the hands. The source of infection is a sick person, while in the case of avian flu – an infected bird. The virus is transmitted through direct contact with a sick person or by touching a dead bird. Eating raw eggs from sick birds and eating undercooked meat can also transmit the infection to humans.
Every several or several dozen years, one cell may become infected with two types of virus, e.g. human and avian. This infection creates a new virus subtype that can cause influenza pandemics. This type of virus variation is called antigen jump and only affects influenza type A 1.
The hatching period for the flu is on average two days, but it can be up to a week. However, the period of infectivity is: 1 day before and 3-5 days after the onset of symptoms (in adults); a few days before and 10 days or less after onset (in children). In turn, immunocompromised people can shed the virus and be a source of infection for up to several weeks / months.
The risk factors that increase the risk of catching flu include:
- lack of proper hand hygiene,
- direct contact with a sick person / animals or contaminated objects,
- being in large groups of people (especially during seasonal flu),
- being in close proximity to a flu patient, without any protection, e.g. face masks,
- touching nose, eyes or mouth with contaminated hands.
Do you want to strengthen your immunity? Try Bio Chlorella algae dietary supplement supporting the immune system.
Flu – symptoms
Flu symptoms are characterized by a sudden onset with fever, runny nose, cough, pain in the head, throat and muscle aches. These general symptoms also include a runny nose and a feeling of crash and weakness. In younger children, the most common symptoms are fever and abdominal pain. Occasionally, vomiting and mild diarrhea are also observed. The flu usually clears up on its own after about 7 days, but some symptoms, such as coughing and general weakness, can last much longer.
- Flu symptoms are keeping you from going, but are you afraid of going to the clinic? Talk to a doctor online!
The fever of flu can be very high, especially in young children. Other types of viruses and bacteria also cause these kinds of ailments, such as the common cold virus and the bacteria that causes angina. It is therefore difficult to diagnose influenza on the basis of symptoms alone.
Flu and colds – differences
Despite the similar clinical picture, there are several differences:
- flu symptoms usually have a rapid onset, while symptoms of a cold begin with a 1-2 day period of general breakdown and weakness (symptoms increase gradually);
- influenza is more often accompanied by high temperature, muscle and joint pain and chills;
- in patients with flu, the runny nose is not so severe; in turn, in people with colds, it is the dominant symptom;
- influenza is a disease that leads to various types of complications, e.g. respiratory failure or pneumonia.
Diagnosis of influenza virus among other infections is necessary in hospitalized patients with complications of influenza, e.g. pneumonia. However, in the rest of the cases it does not matter.
When should a flu patient be hospitalized?
A person suffering from flu requires urgent hospitalization when the following symptoms appear:
- blood plucking,
- pink-colored saliva,
- trouble breathing such as rapid breathing, heavy and noisy breathing, shortness of breath, tightness in the chest or pain in the lungs
- presence of blue or bloody spots on the skin,
- a blueish area around the mouth and direct mouth (including the tip of the nose),
- oliguria – passing urine in much smaller amounts than usual; dry mouth and dizziness;
- episodes of collapsing while trying to get up
- problems with walking and moving hands as a consequence of muscle weakness,
- low blood pressure,
- high temperature (over 40 degrees Celsius),
- delirium,
- letarg,
- loss of consciousness,
- seizures
- disturbance of consciousness and problems with waking the sick person.
Therefore, patients who have high fever for more than 3 days or reappear after a few days of break should consult a doctor as soon as possible. How the flu works and what symptoms accompany it depend on the general condition of the patient before the infection, his age, addictions (e.g. smoking), diet and the properties of the virus. More than half of infections due to the flu virus may be asymptomatic.
The diagnosis of the flu
Most patients do not need tests for influenza virus because the disease is relatively mild and will resolve without treatment. Diagnostic methods are performed on the recommendation of a physician in some patients who are hospitalized due to the severe course of the flu.
Among the auxiliary tests performed in the diagnosis of influenza, the following can be distinguished:
1. Virological examination – including detection of viral DNA material by RT-PCR method; virus isolation on the basis of culture and immunofluorescence method and antigen test in material taken from the throat and nose.
Metoda RT-PCR it is most accurate. The material for testing is taken with a swab made of plastic. What the test result will be depends on several factors:
- method and time of material collection;
- type of material;
- conditions of transport and storage of the material.
Even the smallest of errors can lead to a false-negative result. If there are any doubts about the validity of the test results, repeating the test should be considered. Laboratories that perform RT-PCR testing are located, among others, in Gdańsk, Kraków, Olsztyn, Katowice, Łódź, Białystok, Bydgoszcz, Poznań, Wrocław and Warsaw.
Rapid antigen test for the presence of influenza virus it is characterized by medium sensitivity. Thus, a negative result is not always the basis for excluding the disease. In the case of the A / H1N1v influenza virus, this sensitivity ranges from 10-70%. Virological testing is considered in patients at increased risk for complications or with progressive influenza-like illness.
2. Serological examination – although it does not play a major role in practice, it may mean specific antibodies to the influenza virus. The material for the study is taken from the serum during the acute phase of the disease.
A positive virological test result is the basic criterion of influenza virus infection (in the case of laboratory-confirmed disease). It should be remembered that the symptoms present are not sufficient to make a complete diagnosis, as many other microbes cause similar symptoms. The presence of influenza is most often considered during the endemic season, in every patient with cough and high temperature.
In addition, the classification of the severity of the disease also plays an important role in the diagnosis. Sometimes severe cases and complications are an indication for hospitalization, especially when there are signs of pneumonia or symptoms from the central nervous system (e.g. convulsions, encephalitis). Severe flu is also indicated by an exacerbation of a chronic disease, such as heart or kidney failure or asthma.
Remember that you do not need to go to the clinic to consult your GP while you are ill. You can also visit the National Health Fund online via the halodoctor.pl portal.
Flu should be differentiated from:
- colds and other viral respiratory infections,
- bacterial airway inflammation.
Complications of the flu
Influenza complications usually occur in all patients. A special risk group includes:
- people over 65 years of age,
- children under the age of 5,
- pregnant women (especially in the second and third trimesters),
- overweight / obese people (BMI ≥40),
- people with chronic diseases: heart, lungs, immunodeficiency (e.g. HIV infection), diabetes, congestive heart failure.
Flu complications include:
- secondary bacterial pneumonia and influenza pneumonia (most often caused by H.eamophilus influenzae, Streptococcus pneumonieae and Staphylococcus aureus);
- bronchiolitis (especially in infants and children),
- exacerbation of chronic diseases, e.g. asthma, obstructive pulmonary disease, circulatory system ailments, heart failure, ischemic heart disease,
- streptococcal angina,
- sepsis (rarely),
- very rarely (usually in children) Reye’s syndrome – usually associated with the intake of acetylsalicylic acid preparations.
- myocarditis,
- meningitis,
- muscle inflammation,
- multi-organ failure (rare),
- encephalopathy,
- transverse myelitis.
Influenza complications are very serious, so don’t underestimate your illness! Make an appointment with a doctor online to start treatment as soon as possible
Flu treatment
In people suffering from flu, it is recommended, first of all, to rest in bed, drink plenty of fluids, get plenty of sleep and isolate the patient from the environment. Treatment of this condition has many faces, and the treatment options depend on the condition of the patient (e.g. in pregnant women, start therapy with oseltamivir as soon as possible).
Symptomatic flu treatment includes:
- plenty of bed rest,
- drinking plenty of water
- use of expectorants for a wet cough (e.g. guaiacol) or mucolytic drugs (e.g. bromhexine, acetylcysteine),
- use of antipyretics and painkillers, e.g. paracetamol, ibuprofen (patients under 18 years of age should not be given acetylsalicylic acid because there is a risk of Reye’s syndrome),
- use of antitussive and nasal decongestants, if necessary.
Antiviral treatments include:
The following are active against the influenza virus:
- neuraminidase inhibitors (active against influenza A and B viruses) – oseltamivir and zanamivir,
- M2 inhibitors (active against influenza A virus only) -amantadine and rimantadine.
Before each endemic season, recommendations for antiviral therapy are updated as the resistance of viruses to preparations changes each year.
What are the indications for oseltamivir or zanamivir?
1. Justified suspicion of influenza or its laboratory confirmation in patients who are at increased risk of severe course of the disease and complications. Treatment with these preparations is initiated as soon as the first symptoms appear, regardless of their severity.
2. Confirmation or suspicion of severe influenza or its complications. Treatment with oseltamivir should be started as soon as possible, especially in pregnant women. Lack of improvement leads to an increase in the dose of the drug (in adults it can be as much as 150 mg every 12 hours). When oseltamivir is not available or strains are resistant to this drug, patients will be given zanamivir.
Dosage of oseltamivir in different age groups according to body weight:
- 0-1 months (no information on use in this age group) 2 mg / kg 2 x plot
- 1-3 months 2,5 mg / kg bw 2 x plot
- 3-12 months 3 mg / kg bw 2 x plot
- ≤15 kg mc. 30 mg p.o. 2 x dz.
- 15-23 kg mc. 45 mg p.o. 2 x dz.
- 24-40 kg mc. 60 mg p.o. 2 x dz.
- > 40 kg bw or> 12. 75 mg after 2 x plot
Treatment regimen
- oseltamivir – treatment with this preparation usually lasts 5 days; patients who are unable to swallow tablets can prepare a suspension for oral administration (from the contents contained in the capsule, according to the instructions);
- zanamivir (dry powder inhaler) – is a preparation indicated for use after the age of 5; takes the form of inhalation.
Treatment of hospitalized patients
Hospital treatment is undertaken in patients with severe or progressive flu. After the patient is transported to hospital, an initial assessment is performed:
- X-ray examination – in case of shortness of breath;
- pulse oximeter monitoring of hemoglobin oxygen saturation;
- performing RT-PCR tests for influenza virus; in intubated patients, material is taken from the nose or throat;
- frequent assessment of the patient’s condition (it may worsen at any time).
Immediately after the patient is admitted to the hospital, treatment with an antiviral agent (e.g. oseltamivir) is initiated. It is used until symptoms resolve and the results of virological tests are obtained, which indicate that the virus has replicated. In patients with severe course of influenza who are refractory to treatment with oseltamivir, the inclusion of zanamivir (available only for final import) or ribavirin (also available for import) is considered.
In patients with influenza and coexisting pneumonia, antibiotic therapy should be initiated in addition to antiviral therapy. Antibiotics must not be used prophylactically (unless microbiological tests indicate the bacterial nature of pneumonia). On the other hand, glucocorticosteroids are used only in the case of septic shock (in a low dose). In other circumstances, they pose a risk of side effects, including prolongation of viral replication.
Treatment of cough, runny nose, headaches, muscle aches and throat aches
1. Use painkillers and antipyretics. Paracetamol is considered to be the safest, and should be used as needed in the event of symptoms. Its effect can last up to 6 hours. Attention! Overdosing of the drug can damage the liver.
2. Ibuprofen or naproxen also work well. They have a much stronger effect than paracetamol, but more often lead to side effects such as irritation of the gastric mucosa.
3. For vasoconstriction of the nasal mucosa, local decongestants in the form of xylometazoline or oxymetazoline are recommended. They have properties that improve nasal obstruction. however, they should not be used for more than 5-7 days as they may irritate the nasal mucosa and aggravate the runny nose.
4. Oral nasal decongestants are preparations that contain pseudoephedrine, ie an agent related to amphetamine. Preparations of this type should not be administered to people with arterial hypertension and ischemic heart diseases.
5. Antitussive preparations such as butamirate or levodropropizin are recommended for dry cough. As an alternative, you can use a tablespoon of honey at bedtime.
Treatment of influenza must be supported with appropriate supplements. Large doses of vitamin C can help, so it is worth reaching, for example, Vitamin C 454 g from Swanson. You can also use herbal infusions, such as Ecological gentle herb, which has anti-inflammatory and antibacterial properties. Echinacea also has a strengthening effect on the body, from which you can prepare tea.
Flu and pregnant women
There is an increased risk of complications from influenza in pregnant women. Pregnancy may go unreported, premature delivery may occur or the life of the fetus may be endangered. Therefore, if influenza is suspected in a pregnant woman, careful observation of the patient is necessary, no matter how severe the symptoms of the disease are. In addition, appropriate antiviral treatment should be instituted as soon as possible, even if a laboratory test result has not yet been obtained. In a pregnant woman, the treatment of pain and high temperature should be limited to the use of paracetamol (NSAIDs and acetylsalicylic acid are prohibited in pregnancy). The dose of oseltamivir can be taken up to a dose of 75 mg every 12 hours.
In the case of a nursing woman, it is not necessary to stop breastfeeding during treatment. However, you should maintain hygiene, i.e. wear a face mask during contact with the child and wash your hands frequently.
Seasonal flu vaccines
Vaccines are designed to prevent flu, especially in people who are at higher risk of complications from influenza, such as diabetes or people over 50 years of age). In addition, vaccination is recommended for all people from 6 months of age (to minimize the likelihood of catching the flu). Vaccinations should be performed in the fall, just before the flu season. It is necessary to qualify by a doctor.
After the administration of the vaccine, our body’s immune system begins to produce antibodies, i.e. to defend itself against the disease. Resistance usually develops within three weeks of vaccination and lasts up to 12 months. The vaccine is most effective in healthy adults. The vaccine is valid for one flu season.
Contraindications:
- hypersensitivity to any component of the vaccine,
- acute infections
- complaints with fever.
Are flu vaccines safe?
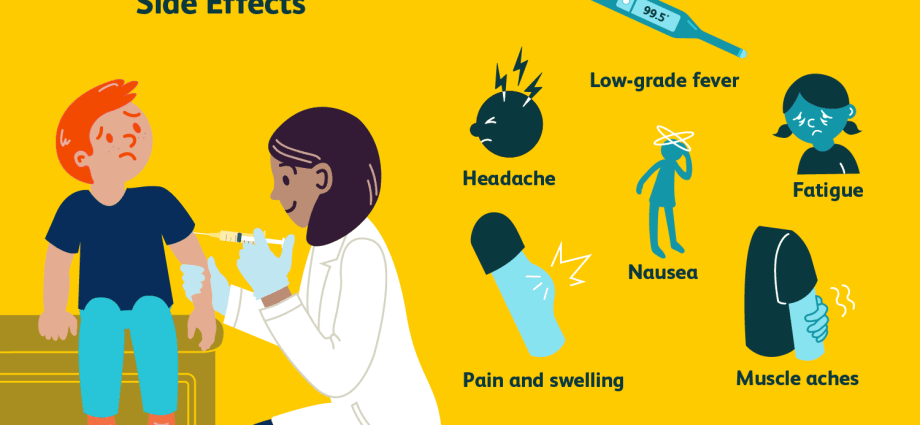
Vaccines have been produced for almost 60 years. Numerous scientific studies and observations after dosing have shown that they are safe for pregnant women, adults, children and chronically immunocompromised people. However, side effects may occur in the form of:
- local reactions: there may be pain and redness at the injection site, usually mild (this reaction will disappear spontaneously in a maximum of two days);
- general response: less than 15% vaccinated people; you experience high temperature, headaches, muscle and joint pains, and a general feeling of being unwell. However, the symptoms are not severe and disappear after about two days. Systemic reactions following administration of the vaccine usually occur in young children who have been vaccinated against influenza for the first time.
Vaccinations are considered to be the best method of flu prevention. Unfortunately, the body does not have resistance to the many types of the influenza virus that arise as a result of mutations in the virus. This variability makes it necessary to change the composition of vaccines every year. However, keep in mind that the vaccine does not completely protect against the flu virus and its complications! Vaccine effectiveness is particularly reduced in the elderly (around 60%). However, it has been shown that vaccinated people were much less likely to be hospitalized for influenza and its complications. It should also be emphasized that influenza vaccines not only protect against infection, but also complications that pose a threat to health and life and the patient.