Contents
- Bronchiectasis: treatments and life expectancy
- What is bronchiectasis?
- Bronchiectasis, congenital and acquired
- What are the causes of bronchiectasis?
- Respiratory infections (diffuse or focal bronchiectasis)
- Mechanical obstructions of the airways (focal bronchiectasis)
- Genetic diseases (diffuse bronchiectasis)
- Immunodeficiencies (diffuse or focal bronchiectasis)
- Systemic diseases (diffuse bronchiectasis)
- Immun-allergic (diffuse or focal bronchiectasis)
- What are the symptoms of bronchiectasis?
- How to treat bronchiectasis?
- Modern treatment tactics
- Rehabilitation, prevention, possible risks
Bronchiectasis: treatments and life expectancy
Bronchiectasis are dilations and destruction of the bronchi due to infection and chronic inflammation. The most common causes include cystic fibrosis, immune deficiencies, and recurrent infections. The most common symptoms are chronic cough, coughing up purulent sputum, fever, and dyspnea. Treatment and prevention of acute attacks includes administration of bronchodilators and antibiotics, removal of secretions, and management of complications such as hemoptysis and other lung damage due to resistant or opportunistic infections.
Bronchiectasias are irreversible morphological changes (expansion, deformation) and functional inferiority of the bronchi, leading to chronic suppurative lung disease. The whole complex of pulmonary and extrapulmonary changes in the presence of bronchiectasis is called bronchiectasis.
What is bronchiectasis?
Bronchiectasis would have been identified for the first time in 1819, by Doctor René-Théophile-Hyacinthe Laennec, inventor of the stethoscope. This is an abnormal dilation of a portion of the bronchi, as a result of irreversible damage to the walls of the airways, causing a build-up of mucus which increases the risk of lung infections. This dilation of the bronchi can affect:
- many regions of the lung: this is called diffuse bronchiectasis;
- one or two regions of the lung: this is called focal bronchiectasis.
Bronchiectasis can develop at any age. Its prevalence increases with age and female sex. All ages combined, it is from 53 to 556 cases per 100 inhabitants and is greater than 000 cases per 200 inhabitants among those over 100 years of age.
The prognosis varies widely. With appropriate treatment and follow-up, people with bronchiectasis have a normal life expectancy. In contrast, people with severe bronchiectasis, concomitant conditions such as chronic bronchitis or emphysema, or complications such as pulmonary hypertension or cor pulmonale tend to have a less favorable prognosis. The prognosis for patients with cystic fibrosis is the most unfavorable, with a median survival of 36 years.
Antibiotics and vaccination programs have greatly reduced the occurrence of bronchiectasis in industrialized countries, while this disease remains common in poor countries.
Bronchiectasis, congenital and acquired
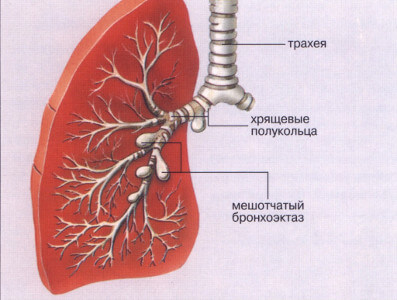 Congenital bronchiectasis is relatively rare and develops due to impaired formation of the bronchial tree. The histological sign of congenital bronchiectasis is a disorderly arrangement of the structural elements of the bronchi in their wall.
Congenital bronchiectasis is relatively rare and develops due to impaired formation of the bronchial tree. The histological sign of congenital bronchiectasis is a disorderly arrangement of the structural elements of the bronchi in their wall.
The main etiological factor of acquired bronchiectasis is a genetically determined inferiority of the bronchial tree (underdevelopment of the elements of the bronchial wall), which, in combination with impaired bronchial patency and the appearance of inflammation, leads to persistent deformation of the bronchi.
The formation of bronchiectasis is largely promoted by whooping cough, acute respiratory infections, measles, bronchitis, pneumonia, lung abscesses, tuberculosis, foreign bodies in the tracheobronchial tree.
Main complaints: cough with a large amount of purulent sputum, hemoptysis, chest pain, shortness of breath, fever, sweating, weight loss and decreased performance. The amount and nature of sputum depends on the degree of bronchial damage. It may contain impurities of blood and pus, an unpleasant odor.
The disease is characterized by exacerbations and remissions. During exacerbations, the temperature rises, shortness of breath, wheezing in the chest, and blue lips appear. Against the background of a long course, the patient’s fingers acquire the characteristic shape of drumsticks, and the nails – of a watch glass. Gradually, the general condition of the patient worsens.
Bronchiectasis is often complicated by pulmonary bleeding, abscess formation, development of pulmonary fibrosis and emphysema, “cor pulmonale”, amyloidosis.
What are the causes of bronchiectasis?
The possible causes of bronchiectasis are very diverse. The most common cause is chronic or recurrent infection, caused by immune system disorders or birth defects that affect the structure or function of the airways and contribute to their obstruction.
Respiratory infections (diffuse or focal bronchiectasis)
These include:
- whooping cough ;
- measles ;
- influenza ;
- tuberculosis ;
- respiratory syncytial virus infections, etc.
Mechanical obstructions of the airways (focal bronchiectasis)
As :
- lung tumor;
- broncholithiasis;
- chronic enlargement of the lymphatic glands;
- inhaled foreign body;
- changes following lung surgery;
- mucus etc.
Genetic diseases (diffuse bronchiectasis)
To know :
- Cystic fibrosis ;
- primary ciliary dyskinesia (PCD), a chronic disease characterized by abnormal lung development from birth;
- alpha-1-antitrypsin deficiency, a disease affecting the lungs and liver.
Immunodeficiencies (diffuse or focal bronchiectasis)
As :
- immune deficiency syndromes such as AIDS;
- l’hypogammaglobulinémie, etc.
Systemic diseases (diffuse bronchiectasis)
These include:
- rheumatoid arthritis;
- ulcerative colitis;
- Crohn’s disease;
- the Sjögren syndrome;
- systemic lupus erythematosus, etc.
Immun-allergic (diffuse or focal bronchiectasis)
To know :
- allergic bronchopulmonary aspergillosis (ABPA), an allergic reaction to a fungus called Aspergillus, most commonly occurring in people with asthma or cystic fibrosis, can cause mucus plugs that obstruct the airways.
Bronchiectasis can also result from inhaling toxic substances causing damage to the bronchi:
- vapors of noxious gases, smoke (including tobacco smoke) or noxious dust such as silica or carbon dust;
- food or stomach acid.
What are the symptoms of bronchiectasis?
Symptoms usually start insidiously and tend to worsen gradually over the years, accompanied by episodes of acute worsening.
These include:
- a chronic cough, the most common symptom, which usually occurs in the early hours of the morning and late in the day and produces thick, profuse and often purulent sputum. The volume of this sputum can vary considerably, as well as its color (white, yellow, green, dark green or brown);
- difficulty breathing (dyspnea);
- shortness of breath;
- a hissing sound produced by the movement of air in the airways (wheezing);
- pleural-like chest pain;
- relapsing fever;
- severe fatigue;
- a decrease in the amount of oxygen carried in the blood (hypoxemia);
- pulmonary arterial hypertension;
- right heart failure;
- coughing up blood (hemoptysis).
Acute exacerbations are common and may be due to a new infection or to a worsening of an existing infection. Acute flares of the disease are marked by worsening coughing, increased dyspnea, as well as the volume and purulence of sputum. If the bronchiectasis is severe and chronic, there is usually weight loss.
How to treat bronchiectasis?
With the right treatment, people with bronchiectasis can remain stable for many years and control their symptoms well. The treatment of bronchiectasis aims to:
- prevent exacerbations;
- treat symptoms;
- improve the quality of life;
- prevent the worsening of the disease.
Prevention of exacerbations
- regular vaccinations such as the annual influenza and pneumococcal vaccination which provides protection against the most common bacterial cause of pneumonia;
- airway clearance measures;
- macrolide antibiotics.
Treatment of symptoms
- antibiotics;
- inhaled bronchodilators;
- airway clearance measures (mucolytic drugs);
- inhaled or oral corticosteroids;
- in rare cases, surgical removal of part of the lung if the bronchiectasis affects only a small part of the lung or if part of the lungs have severe lesions that lead to recurrent infections or emit a large amount of blood when coughing;
- oxygen therapy if necessary to avoid complications such as cor pulmonale;
- embolization of the bronchial arteries in the event of hemoptysis.
Improved quality of life
- respiratory physiotherapy (postural drainage, chest percussion) to promote drainage of secretions and mucus;
- regular physical activity to eliminate sputum and promote better lung function;
- Healthy eating ;
- humidifying the air and inhaling salt water to relieve inflammation and mucus buildup;
- respiratory functional rehabilitation sessions to improve physical resistance and reduce the effects of symptoms and the physical and emotional impact on daily life.
Prevent the worsening of the disease
- smoking cessation aids;
- vaccination ;
- antibiotics.
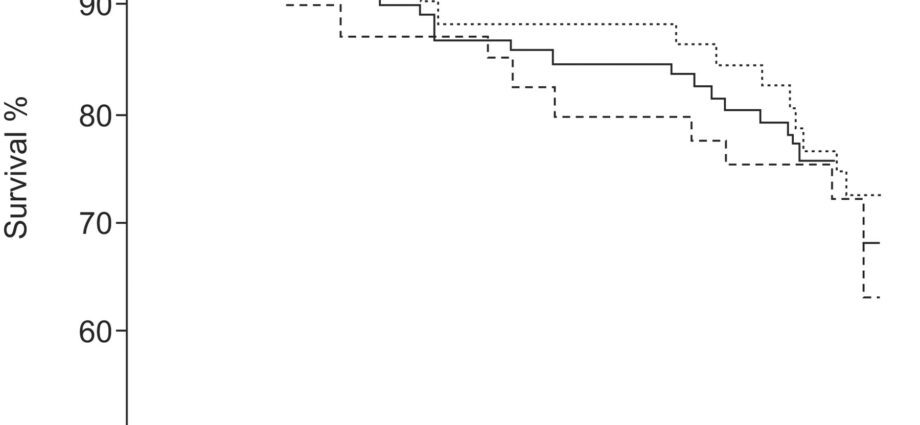
Advanced bronchiectasis in some people, mainly those with advanced cystic fibrosis, can be treated with a lung transplant. The 5-year survival rate is between 65% and 75% for heart-lung transplantation or both lung transplantation. Lung function usually improves within 6 months and improvement can continue for at least 5 years.
Modern treatment tactics
При бронхоэктазе назначают современные антибиотики класса макролидов, чтобы подавить патогенную микрофлору, и β2-агонисты для устранения рефлекторных спазмов мелких бронхов. Также эффективны муколитики, разжижающие слизь и облегчающие ее откашливание. Чтобы купировать воспаление, при лечении бронхоэктаза показаны гормональные средства. Для активизации собственных защитных сил организма в терапевтическую схему включают иммуностимуляторы.
Ключевая процедура консервативного лечения бронхоэктаза — санация бронхиального древа (очистка просвета бронхов от гнойной мокроты с последующим введением антибиотиков). При признаках кислородной недостаточности назначают кислородотерапию. Больному также назначают комплекс упражнений, способствующих эвакуации бронхиальной мокроты, и вибрационный массаж грудной клетки. Для общего укрепления организма показаны:
- high-calorie diet – 3000 kcal per day;
- diet therapy – functional nutrition rich in nutrients;
- vitamin therapy.
Given the irreversibility of the process, and, consequently, the futility of conservative therapy, the only radical method of treating bronchiectasis should be considered surgical, the volume of which depends on the spread of bronchiectasis.
Rehabilitation, prevention, possible risks
An important component of complex rehabilitation for bronchiectasis is lifestyle correction. The patient needs to walk in the fresh air, stop smoking and avoid passive smoking, eat a balanced diet, exercise, and do breathing exercises regularly.
It is important to be registered with a pulmonologist, attend preventive appointments with the frequency prescribed by the doctor, and, if necessary, take courses of physiotherapy. Comprehensive prevention provides for timely treatment of respiratory diseases and hardening.
Without adequate treatment of bronchiectasis, chronic bronchitis, pulmonary and heart failure, cor pulmonale, and bronchial asthma develop. Patients experience reduced performance and poor quality of life. It is extremely important to consult a doctor in a timely manner in order to achieve a long-term stable remission.