Contents
Achalasia: all about esophageal achalasia
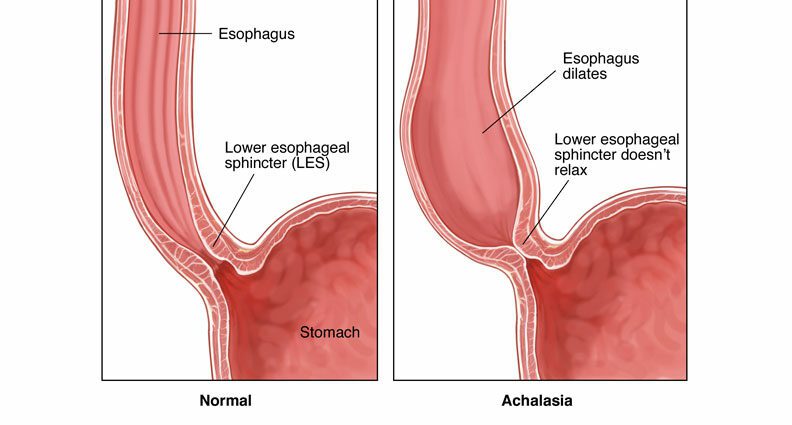
Achalasia is a disorder that occurs when esophageal contractions are absent or abnormal, the lower esophageal sphincter does not relax normally, and the resting pressure of the lower esophageal sphincter is increased. The goal of treatment is to relieve symptoms by dilating the lower esophageal sphincter, by injecting botulinum toxin, with a balloon, or by severing the muscle fibers of the sphincter.
What is achalasia?
Achalasia, also called cardiospasm or megaesophagus, is a movement disorder of the esophagus, which is characterized by a feeling of discomfort when swallowing. It is a rare disease, having a prevalence of 9-10 / 100 people. It can appear at any age, both in men and in women, with a peak in frequency between 000 and 30 years. It usually begins, in a sneaky way, between the ages of 40 and 20 and gradually evolves over several months or even years.
What are the causes of achalasia?
Once swallowed, food travels to the stomach through rhythmic esophageal muscle contractions called peristalsis. Then food enters the stomach through the opening of the lower esophageal sphincter, which is a muscle ring that holds the lower end of the esophagus closed, so that food and stomach acid do not flow back up. into the esophagus. When you swallow, this sphincter relaxes normally to allow food to pass into the stomach.
In achalasia, two abnormalities usually appear:
- the absence of esophageal contraction, or aperistalsis, caused by degeneration of the nerves in the wall of the esophagus;
- and the absence or incomplete opening of the lower esophageal sphincter.
What are the symptoms of achalasia?
The main symptom of achalasia is swallowing disorders. This leads to:
- dysphagia, that is, a feeling of food blockage when swallowing or as it passes through the esophagus, which is present in 90% of people with achalasia;
- regurgitations, especially during sleep, of undigested food or liquids, which stagnate in the esophagus, are present in 70% of cases;
- sometimes constricting chest pain;
- if patients inhale food into the lungs, it can result in a cough, an infection of the respiratory tract, bronchiectasis ie dilation of the bronchi, or inhalation pneumonia.
These symptoms can persist for many years, intermittently and capriciously, and occur with solid foods and / or liquids. They can gradually worsen and lead to slight to moderate weight loss or even undernutrition. Respiratory complications are common, affecting 20 to 40% of patients.
How to treat esophageal achalasia?
The diagnosis of achalasia is based on:
- an oesopastro-duodenal endoscopy exploration which allows to observe the lining of the esophagus;
- an x-ray examination of the esophagus, in which the patient ingests barite, an X-ray opaque contrast medium, which makes it possible to visualize a dilated esophagus that does not empty well;
- and finally an esophageal manometry, which makes it possible, thanks to a probe, to measure the pressures along the esophagus and the degree of relaxation of the lower esophageal sphincter. In the event of achalasia, manometry notes the absence of esophageal contractions in response to swallowing of water as well as a total or incomplete absence of relaxation of the lower esophageal sphincter.
No treatment can correct the pathophysiological alterations responsible for achalasia.
The proposed treatments aim to relieve symptoms by reducing the pressure of the lower esophageal sphincter and improving the passage of esophageal contents to the stomach through a gravity effect:
- the injection of botulinum toxin into the lower esophageal sphincter by endoscopic route allows it to be released. This treatment, renewable every six to twelve months, is mainly indicated in the most fragile patients at high surgical risk;
- endoscopic dilation, or pneumatic dilation, using a balloon placed at the esogastric junction that is inflated, and which allows to stretch the muscles and promote emptying of the esophagus. It is effective in nearly 80 to 85% of cases;
- surgical myotomy, known as Heller’s, consists of cutting the muscle fibers of the lower esophageal sphincter by laparoscopy, a surgical technique allowing access to the interior of the abdomen through small incisions . This intervention, effective in more than 85% of cases, is generally associated with the creation of a valve at the level of the esogastric junction to limit the risk of gastroesophageal reflux;
- the more recent peroral endoscopic myotomy (POEM) is an incision made endoscopically. This technique, effective in 90% of cases, consists of creating a tunnel in the wall of the esophagus in order to directly access the lower esophageal sphincter to cut it.
Certain pharmacological treatments can help relax the sphincter. They have limited effectiveness but can prolong the time between two balloon dilations or botulinum toxin injections. They can be considered in patients with a contraindication to surgery or endoscopic dilation, and in the event of failure of treatment with botulinum toxin. These include in particular:
- nitrates, such as isosorbide dinitrate, to be placed under the tongue before meals; improvement of symptoms is observed in 53-87% of cases;
- calcium channel blockers, such as nifedipine, also placed under the tongue 30 to 45 minutes before a meal. Improvement in dysphagia is reported in 53 to 90% of cases.