What is head trauma?
If the expression “head trauma” (TC) literally corresponds to a shock to the skull, whatever its intensity, in medical terms, head trauma corresponds to a shock the intensity of which causes a disturbance of consciousness, even briefly. . Many life circumstances can lead to head trauma (sports, professional, car or public highway accident, domestic accidents, assault, fall, blow to the head, firearm, etc.).
SOME ESSENTIAL CONCEPTS
- Cerebral inertia
Head trauma can be mild or severe, with all possible intermediaries. Its severity depends on the existence of intracerebral lesions or the existence of an extra-cerebral hematoma, bleeding located between the skull and the brain. From a functional point of view, brain damage is linked to acceleration-deceleration mechanisms (the most dangerous) responsible for stretching, crushing and shearing forces within the brain itself. These forces can stretch neurons (brain cells) and their axonal extensions (“cables”). Indeed, the heavy brain of nearly 1400 grams has its own inertia, especially since it is not attached directly to the bone of the skull. In a sufficiently violent impact, the brain strikes the inside of the skull back and forth, or to the sides, like the human body subjected to sudden acceleration or deceleration, such as a frontal accident in a car. . The two mechanisms are often associated by a phenomenon of blow and kick.
- Initial loss of consciousness
Equivalent to a knockout, a major shaking of the brain will cause cerebral astonishment, responsible for the loss of consciousness, and likely to trigger brain damage or a hematoma. In general, the faster the return of consciousness, the greater the chances of a return to normal without after-effects. On the other hand, a deep and lasting loss of consciousness is more worrying and may correspond to the existence of brain damage. However, a rapid return to normal is not sufficient to formally rule out the existence of a brain injury. Consequently, any initial loss of consciousness in the context of trauma should be considered as a sign of seriousness, until proven otherwise, and lead to close clinical monitoring, even in the absence of visible brain damage to the patient. CT scan or MRI. But beware, the absence of initial loss of consciousness can not be considered as the mark of a benign TC either. Indeed, According to a large study, this initial loss of consciousness may be missing in 50 to 66% of cases where the scanner finds an intracranial lesion.
- Skull fracture
The severity of a head injury does not just depend on whether or not a skull fracture exists. Clearly, a fracture visible on the x-ray should not be the only parameter of severity of a head trauma, which is why it is not performed systematically. Indeed, if the fracture of the skull shows a severe trauma, sufficient to break the bone, in itself it does not require any particular treatment other than analgesics to calm the pain. One can therefore suffer from a skull fracture without any associated brain damage or hematoma. One can also suffer from a serious intracranial hematoma, and this, in the absence of fracture of the skull. Some even consider that the fracture corresponds to the dissipation of the shock wave which will fade on the surface instead of spreading deep into the brain, thus protecting the underlying brain structures, like the shell. of an egg. However, the observation of a fracture line, particularly at the temporal level, should encourage caution because of an increased risk of developing an extra-dural hematoma (risk multiplied by 25).
Several types of lesions
- Extracerebral hematomas
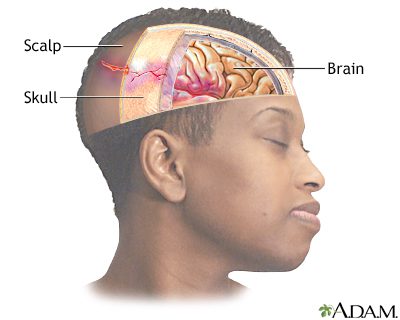
Located between the internal face of the skull and the surface of the brain, these extra-cerebral hematomas correspond to blood collections most often linked to the tearing of the fine venous vessels supplying the three membranes enveloping the brain (the meninges) which are located just under the skull bone. Acceleration-deceleration phenomena can cause these tears. These three meninges constitute a cerebral protection which is insufficient in the event of significant trauma.
In practice, we distinguish:
· The so-called “subdural” hematomas, located between two meninges (the arachnoid and the dura, the outermost). Linked to venous tearing or the consequences of a cerebral contusion, the subdural hematoma can occur immediately after the head trauma (immediately coma) or later. Surgery is essential in the majority of cases when there is a risk of compression of the brain. It consists in evacuating the hematoma.
· The extra-dural hematomas, located between the inner surface of the skull bone and the dura. Especially temporal, extra-dural hematomas are linked to the existence of a lesion of the middle meningeal artery. With some exceptions (extra-dural hematoma of very small volume and well tolerated by the patient), this type of hematoma requires emergency intervention (trepanation) intended to evacuate this collection of blood which also threatens to compress the brain.
- Intracerebral lesions
They include several types of attacks, local or diffuse, which can be associated and which make all the difficulty of the prognosis. Each head trauma is specific.
A head trauma can therefore be accompanied in a fraction of a second by:
· Bruises on the surface of the brain. They correspond to injuries resulting from contact of the surface of the brain with the internal face of the bone of the skull, despite the meninges. Contusions affect the front of the brain as well as the back (return shock) and the temporal area. Hematoma, necrosis at the site of bleeding, edema or small hemorrhages on the surface of the brain are possible.
· Damage to neurons, or axonal damage. Indeed, the two very distinct layers constituting the brain and called white substances (in the center) and gray (covering the white substance on the outside), do not have the same density and therefore, a different inertia. During an impact, the zone of separation of the two layers will be stretched or sheared, causing damage to the neurons passing through it.
Or postponed after several minutes or hours, by:
· Edema, in other words an accumulation of water which will increase the pressure inside the brain and this, around the lesion in the hours following the accident, with the risk of developing intracranial hypertension and repression the mass of the brain on the opposite side (so-called “engagement” syndrome).
· Ischemia, very feared, in other words a decrease in oxygen in the brain tissue linked to a decrease in vascularization, following the accident or the development of compressive edema. A cascade of biochemical reactions can lead to the cell death of the neurons involved.
· Intracerebral hemorrhages (hematomas)