Contents
What is blepharitis?
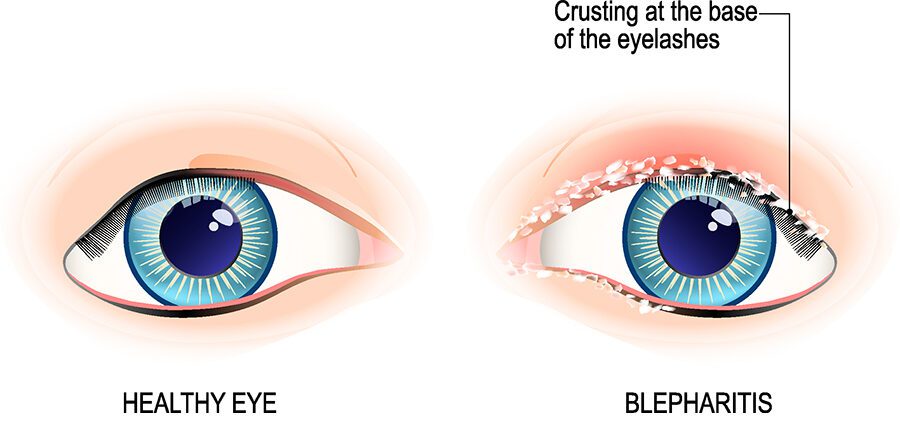
Blepharitis is an inflammation of the free edge of the eyelid (the pinkish red rim located at the level of the eyelashes). This inflammation can spread to the skin (the eyelid), the inside of the eyelid, located against the eye, or even the eye itself. It can cause eyelash loss called madarosis.
Symptoms of the disease
Blepharitis causes redness of the eyelid margin. Sometimes there are crusty deposits at the base of the eyelashes. In very inflammatory forms, there may be eyelid edema, deformities or ulcers at the edge of the eyelids.
It is accompanied by sensations of a foreign body, burning, itching, even pain and more rarely a decrease in visual acuity.
Causes of blepharitis
1 / Staphylococcus
Blepharitis linked to staphylococcus is either recent and sudden onset, or it complicates blepharitis of another cause by manual contamination.
Inflammation of the free edge of the eyelid is marked, often accompanied by erosions of the ciliary follicle, hard crusts around the root of the eyelashes, frill scaling around the eyelash, then eyelash loss (madarosis) and an irregularity of the eyelid margin (tylosis)
2/ Demodex
Demodex folliculorum is a skin parasite that lives in the hair follicles of the face. It can lead to demodecidosis of the face (a rash that looks like rosacea but does not heal with antibiotics).
In blepharitis related to demodex overgrowth, the parasites can be seen with the naked eye, which swarm in the form of clear tubular sleeves around the base of the eyelashes.
3 / Rosacea
Rosacea is a pathology giving rosacea and pimples of the cheeks and nose. This pathology is often accompanied by blepharitis since it is found in 60% of cases of cutaneous rosacea. It is even indicative of rosacea when there are no skin signs yet in 20% of cases.
Blepharitis of rosacea is accompanied by posterior involvement, that is to say concerning the mucous side of the eyelid with involvement of the meibomian glands, glands located on the conjunctiva, which are dilated, give out an oily liquid if you press on it and make the tear film greasy. Sometimes these glands are blocked by an oily plug and ignite (meibomite)
The conjunctiva is red, with dilated vessels, swollen areas and it may even in advanced stages have atrophic scars.
4 / Seborrheic dermatitis
Seborrheic dermatitis causes dry redness predominantly in the seborrheic areas of the face (edges of the nose, nasolabial folds, around the eyes, etc.). It can be accompanied by a slightly inflammatory blepharitis, with damage to the eyelid by dermatitis, with fatty scales
5 / Rare causes
The other causes of blepharitis are psoriasis (appearance similar to seborrheic dermatitis), contact or atopic eczema (resulting in eyelid eczema), cicatricial pemphigoid, drug eruptions, chronic lupus, dermatomyositis and body phtiriasis (“Crabs” which can colonize the eyebrows and eyelashes in addition to pubic involvement).
Medical treatments for blepharitis
1 / Staphylococcus
The doctor uses eye drops or ointments based on mercury oxide (twice a day for 7 days: Ophtergine®, Yellow mercuric oxide 1 p. 100 Chauvin®), bacitracin (Bacitracine Martinet®), chloramphenicol (Chloramphenicol Faure® single-dose, one drop 3 to 6 times a day), aminoglycosides (Gentalline® eye drops or ointment, Tobrex® eye drops or ointment, 3 applications / day)
The ointment can be used in addition to eye drops and will then be applied in the evening. It allows the softening of the crusts.
There are antibiotic eye drops based on fluoroquinolones, which are more expensive and more rarely used. Likewise, cyclins are rarely used due to the resistance of many strains of staphylococci.
The simultaneous use of corticosteroids and an antibiotic (Gentasone® ointment) is controversial, but it allows a faster improvement in functional symptoms than the antibiotic alone: local corticosteroid therapy should be used with great care, once the diagnosis of infectious keratitis (herpes…) was formally ruled out by an ophthalmologist.
2/ Demodex
Treatment involves the application of 1% mercury oxide ointment. 100 (Ophtergine®, Yellow mercuric oxide 1 p. 100 Chauvin®), solutions of boric acid (Dacryosérum® single dose, Dacudoses®) and mechanical removal of ciliary sleeves with forceps.
3 / Rosacea
Removal of oily secretions from the meibomian glands
The doctor recommends massaging the eyelids twice a day in order to evacuate the oily secretions from the meibomian glands. This massage can be preceded by the application of compresses soaked in hot water which soften the secretions.
Fight against dry eye
Use of artificial tears without preservative (Gel-Larmes® single dose, 2 to 4 times per day, Lacryvisc® single dose, ophthalmic gel).
Treatment of rosacea
The dermatologist uses oral antibiotics (cyclins: Tolexine®, 100 mg / day for 12 weeks) which have a good impact not only on cutaneous rosacea but also on blepharitis.
Local cyclins such as oxytetracycline (Tetranase®) have no Marketing Authorization in this indication but they can also be effective.
Metronidazole gel at 0,75 p. 100 (Rozex gel®) can be applied once a day to the skin surface of the eyelids and their free edge for 12 weeks.
4 / Seborrheic dermatitis
Hygiene care is again important, in order to eliminate fatty crusts and scales which constitute a source of bacterial proliferation and irritation by using an eyelid cleansing product (Blephagel®, Lid-Care®…).
Blepharitis linked to seborrheic dermatitis is often contaminated with staphylococci, so it requires treatment similar to staphylococcal blepharitis.
Our doctor’s opinion
Blepharitis is most often a benign pathology (apart from staphylococcal disease) but disabling and bothersome on a daily basis. It is often a sign of a dermatological disease (mucocutaneous staphylococcal carriage, rosacea, seborrheic dermatitis, demodecidosis, etc.) that the dermatologist must treat effectively in addition to the care provided by the ophthalmologist. It is therefore a borderline pathology for these two specialists who must act together to relieve patients. Dr. Ludovic Rousseau, dermatologist |
Landmarks
Dermatonet.com, information site on skin, hair and beauty by a dermatologist
www.dermatonet.com
More information on the red eye: http://www.dermatonet.com/oeil-rouge-yeux-rouges.htm/
Writing : Dr. Ludovic Rousseau, dermatologist April 2017 |










Маш олон ийм шинжтэмдэгтэй нүдний зовхины өрөвсөл “асуудалтай хүмүүс зөндөө байдаг тэд гэхдээ энэ талаар сайн мэддэггүй Өрхийн эмч нар л сайн зөвлөх хэрэгтэй … ерөндөг байдаггүй тус хувь хүн өөртөө анхаарал тавих нь чухал….