Contents
- Cracking or rupture of the water pocket, what is the difference?
- Is a discharge still amniotic fluid?
- How is the rupture of the water bag diagnosed?
- When can the water bag rupture during pregnancy?
- Are there any factors that favor the rupture of the water bag?
- Rupture of the water bag: the consequences for the baby
- Rupture of the water bag: a risk for the mother?
- What happens once the pocket of water is broken?
Cracking or rupture of the water pocket, what is the difference?
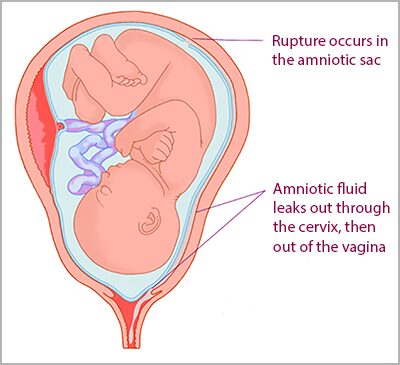
Most often, the amniotic membranes (amnion and chorion) which constitute the bag of water tear very close to the internal opening of the neck, the flow is then frank and relatively abundant. Sometimes the rupture takes place higher, and the quantity of liquid which escapes is less important. That’s what we call a cracking of the water bag. In some very exceptional cases, the breach may become blocked, but generally once the water bag is opened, nothing can prevent the amniotic liquid result.
Is a discharge still amniotic fluid?
Moms-to-be sometimes have a little trouble identifying a fluid leak, especially when it starts with a few drops. Amniotic fluid can be mistaken for urine loss or a vaginal discharge, common during pregnancy. To help you tell the difference, put on a sanitary napkin. Unlike urine, amniotic fluid is colorless or slightly whitish (a bit like lightly soapy water). Its smell is stale and the flow is permanent. With changes in position or coughing, it tends to increase. Sometimes the flow is clear but does not recur. It may be the rupture of an amnio-chorionic pocket. This effusion of liquid is formed between the two membranes, but since the opening only concerns the outermost membrane, the baby remains protected.
How is the rupture of the water bag diagnosed?
In the maternity ward, the midwife will examine you. If the fluid loss is not obvious, she will place a speculum and be able to visualize the amniotic fluid that escapes from the external opening of the cervix. When it is a high (cracking) or old breakage, the flow may be more difficult to confirm. Fortunately, specific biological tests exist.
The simplest (but there are others) can be done during the exam, and the result is immediate. It is based on the pH. That of the vagina is acidic (between 4,5 and 6) while that of the amniotic fluid is basic (7 to 7,5). A kind of large cotton swab is introduced into the vagina. In the presence of amniotic fluid, it changes color from yellow to blue. THE’scan can also help with diagnosis. It shows the amount of amniotic fluid remaining and allows its evolution to be followed.
When can the water bag rupture during pregnancy?
Fortunately, most often the rupture takes place at term, during labor, and allows the birth of a healthy baby. In 5 to 10% of pregnancies, the water bag ruptures before the onset of labor: we then speak of premature rupture of the water bag (RPM). In a third of cases, it appears in a future mother who is not at term (before 37 weeks) and can have harmful consequences on the fetus, mainly in connection with prematurity. The risks for the unborn baby and the action to be taken then vary according to the age of the pregnancy.
Are there any factors that favor the rupture of the water bag?
Bacterial infection plays an important role. It is found in about 40% of ruptures. Moms who have a history of preterm labor or premature rupture of membranes are also at greater risk. It is the same for those who have problems with the cervix (open bite, exposure to Distilbene®, cerclage) or if the position of the placenta is abnormal (placenta previa). Uterine overdistension is also incriminated for example in the event of multiple pregnancies, or too much amniotic fluid (hydramnios). Deficiencies in iron, zinc and vitamin C which weaken the membranes can also interfere. Likewise tobacco or drug use.
Rupture of the water bag: the consequences for the baby
The consequences for the unborn child depend on the precocity of the rupture. They are more numerous and serious if the pregnancy is young. The rupture would also be responsible for 30 to 40% of premature deliveries. According to studies, 6 out of 10 pregnant women give birth in the week following the rupture when it occurs at 29 weeks.
In addition to the problems (especially pulmonary and neurological) linked to an early birth, the risks to the fetus are also infectious. As the baby is now in contact with the outside environment, microbes can colonize the amniotic fluid. We then speak of chorio-amnionitis. A neonatal infection can also declare itself. Finally, too much fluid leakage can cause oligoamnios. This occurs when the production of liquid is no longer sufficient to cover the losses. In early pregnancy, this complication can interfere with the development of the baby and lead to severe malformations.
Rupture of the water bag: a risk for the mother?
The dangers are less serious than in the future baby. It is mainly an infection in the uterus. They are found in 10 to 20% of patients. In addition, when the pocket of water breaks prematurely the cesarean section rate is higher.
What happens once the pocket of water is broken?
Any fluid loss during pregnancy should prompt you to consult. If the rupture of the water bag is confirmed, you will be hospitalizede. Fortunately, strict bed rest is no longer recommended and you can get up to go to the bathroom or take a few steps in your room. Hospitalization at home is sometimes considered on a case-by-case basis after the first check-ups, but it depends on the term of the pregnancy and the obstetric conditions.
- Between 24 and 34 weeks, the future mother will benefit fromcorticosteroid injections. These are essential to increase the pulmonary maturity of the baby and limit complications related to prematurity. If necessary, to allow the corticosteroid course to be completed and to prevent childbirth, a anti-contractions treatment will be in place for 48 hours. Finally, to treat or prevent an infection, the mother will receive antibiotics. The birth will be decided in a center with a neonatal unit in front of any suspicious sign of infection or fetal distress.
- Between 34 and 37 weeks, only antibiotics will be prescribed. Obstetric management is very complex. Obstetricians and pediatricians must weigh two important risks: prematurity and infection, and make the decision to wait with the slightest sign of fetal distress and infection, or to deliver a premature baby to avoid infectious complications.
- At term, it is better that the mother gives birth without waiting too long. Either labor begins spontaneously (this is the case for 8 out of 10 pregnant women at the end of pregnancy) or it is triggered artificially after 12 to 24 hours of rupture.