Contents
Pulmonary hypertension
Do you suffer from shortness of breath on exertion without any cause having been identified? It can be pulmonary hypertension, a severe and serious condition when it takes the form of pulmonary arterial hypertension, which can lead to heart failure.
Pulmonary hypertension, what is it?
Definition
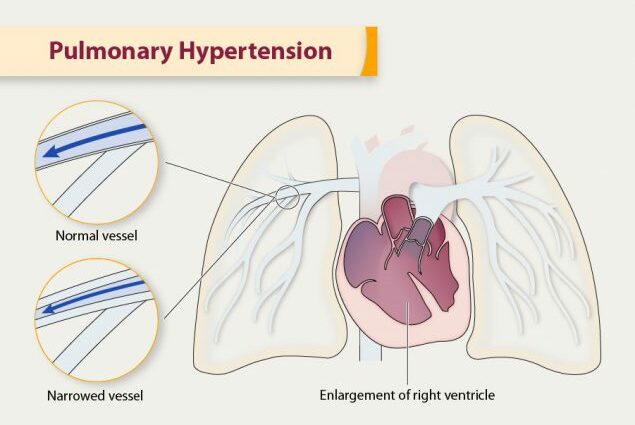
Pulmonary hypertension (HTP) is a disease characterized by abnormally high blood pressure in the small pulmonary arteries, which opposes the flow of blood to the lungs. To compensate, the heart’s right ventricle, which sends blood to the lungs for re-oxygenation, must work harder. When it is no longer successful, respiratory discomfort on exertion appears. At an advanced stage, the patient can develop heart failure, which is fatal in the short term if it is not taken care of.
Causes
Pulmonary hypertension may or may not be associated with various conditions, in particular cardiovascular or pulmonary. Specialists distinguish five forms of the disease involving different mechanisms, corresponding to different causes.
Group 1: pulmonary arterial hypertension, or PAH. This rare and severe disease can be fatal within a few years. It is due to a remodeling of the lining of the pulmonary arteries, causing it to thicken. It often occurs without an identified cause (idiopathic PAH) or in a hereditary context (familial PAH), but can also be linked to certain diseases such as congenital heart problems or HIV infection. It can also be induced by drugs or toxins.
- Group 2: pulmonary hypertension due to left heart disease.
- Group 3: pulmonary hypertension associated with respiratory diseases and / or hypoxia (lack of oxygen supply to tissues). It results, for example, from chronic obstructive pulmonary disease (COPD), respiratory sleep pathologies or developmental abnormalities.
- Group 4: pulmonary hypertension linked to chronic thromboembolic disease. It is the obstruction of the vessels by a blood clot that is the cause.
- Group 5: other causes: sarcoidosis, tumors compressing the vessels, chronic kidney disease, etc.
Diagnostic
Diagnosis is based on a battery of tests that assess how well the heart and lungs are working.
Cardiac echo-doppler
If pulmonary hypertension is suspected, cardiac ultrasound is performed to highlight the elevation of pulmonary arterial pressure and certain cardiac abnormalities. It allows you to directly observe the structures of the heart and their functioning. Coupled with Doppler, it provides visualization of blood circulation.
Cardiac catheterization
Cardiac catheterization is used to clarify the diagnosis. It is performed using a long flexible tube (catheter) inserted into a vein, which goes up to the heart and then to the pulmonary arteries. This test measures blood pressure in the atria, pulmonary artery pressure and blood flow.
Various other examinations are useful for the initial assessment:
- Six-minute walk test (to assess the extent of respiratory discomfort)
- Functional respiratory tests
- X-ray of the lungs
- Electrocardiogram
- Chest scanner (computed tomography)
- Blood tests …
The people concerned
Given the diversity of the causes and forms of the disease, it is difficult to draw a general picture of the people affected by pulmonary hypertension.
In Europe, it is estimated that pulmonary arterial hypertension (PAH) affects about 15 people in a million and up to 50 people in a million if we take into account the underdiagnosis. Anyone is susceptible to the disease. However, it is more common in women aged 30 to 50 (European lung foundation).
In France, 40,5% of new cases of PAH are thought to have no identified cause (idiopathic PAH) and 2,5% have a genetic origin (Pulmonary arterial hypertension in France: results from a national registry. M. Humbert et al., American Journal of Respiratory and Critical Care Medicine, May 2006.).
Symptoms of pulmonary hypertension
Dyspnea on exertion (shortness of breath on exertion)
Pulmonary hypertension is expressed by shortness of breath on exertion. At the beginning, the respiratory discomfort manifests itself during a little sustained effort (climbing the stairs…). Then the daily physical activities become difficult, and soon the breath runs out at the slightest movement.
This shortness of breath can cause discomfort (dizziness, vertigo, etc.).
Tiredness
Affected subjects are very fatigable due to the poor supply of oxygen in the blood.
As the disease progresses, various other symptoms may appear:
- edema of the feet and ankles (related to the development of right heart failure)
- feeling of tightness in the chest
- heart rhythm disturbances, palpitations
- cough (rarely bloody) …
Treatments for pulmonary hypertension
Pulmonary hypertension requires lifelong follow-up. The therapeutic strategy is based on treating the cause. In the absence of an identified cause, the prognosis is poorer because there is no cure. However, thanks to significant progress in recent decades, various treatments now make it possible to relieve the symptoms of the disease and to slow its progression.
Drug treatments
- Vasodilators (calcium channel blockers, prostacyclin and its analogues, etc.), which dilate blood vessels, improve quality of life but are not effective in all patients.
- Anticoagulant drugs are used to prevent the risk of blood clots forming.
- Diuretic treatments are prescribed in case of edema of the lower limbs.
In 2018, a French team discovered that the NMDA (N-Methyl-D-Aspartate) receptor plays a role in the remodeling of the vascular wall. It could constitute a new therapeutic target (http://www.cnrs.fr/insb/recherche/parutions/articles2018/s-cohen-kaminsky.html).
Oxygen therapy
Oxygen supplementation helps improve symptoms associated with poor blood oxygenation.
Lung or cardiopulmonary transplantation
It is the last resort when PAH can no longer be controlled with medication, but can only be attempted in patients who are healthy enough to withstand this heavy surgical procedure.
Therapeutic education and lifestyle adaptation
Physical activity
Limitation of physical activity is necessary: sports practices leading to symptoms of the disease should be avoided. However, regular, low-intensity activity such as walking, adapted to the severity of the disease, may be beneficial.
Diet and lifestyle
A diet without salt, or low in salt, is usually put in place to fight against the problems of pulmonary edema and lower limbs.
Stopping smoking helps improve overall lung function, which helps alleviate symptoms of the disease.
Situations to avoid
Stays at altitude are strongly discouraged due to the reduction in oxygen levels in the air.
Pregnancies are contraindicated, as are unnecessary surgical procedures, as they can suddenly worsen heart problems.
Prevent pulmonary hypertension
Most often, prevention is not possible. However, in people with chronic thromboembolic disease, taking anticoagulants can help prevent blood clots that cause pulmonary hypertension.
Influenza and pneumococcal vaccinations are recommended to avoid worsening symptoms.










Moj brat Vladimir Rakić rođen je 1963. godine, sa srčanom manom: ASD, VSD, Sy. Eisenmengeri. Kateterizacijom srca 1980. utvrđeni su pritisci u plućima previsoki za operativnu korekciju srčane mane. Od 1983. do 1985. lečen je ,,kaptoprilom”, ,,persantinom” i još nekim lekovima, u početku uspešno, ali kasnije mu se stanje pogoršalo. Decembra 1985. rečeno mi je da medicina više nema načina za njega, kako se i potvrdilo 1986, sa pokušajem infuzije prostaglandina PGE1. Međutim, on je od 1987. do 1991. zimovao na moru, što mu je pomoglo jer se podvrgavao hotelskom i kućnom redu i restoranskom radnom vremenu. Inače je mnogo vremena provodio u zadimljenim prostorijama na kompjuterskim igrama, ili se kod kuće bavio njima i danju i noću, hraneći se samo uveče, ,,eurokremom” i ,,koka-kolom”. Tako je do 1990. njegovo stanje postalo kritično – pešačenje, podsticaj srcu, postajalo je sve napornije usled gojaznosti i otoka gležnja i cele potkolenice desne noge; pojavila se i prva epistaksa. On je verovao u Boga, a ja nisam, ali sam se ipak pomolila, i Bog je pomogao, i to vrlo precizno. Naime, tražeći leka, našla sam u “Excerpta Medica” podatak da je prosečno preživljavanje posle transplantacije srca i pluća oko osam godina – tačno toliko mu je prvi put produžen život – od 1991. do 1999. Počeli smo sa makrobiotikom, koja zabranjuje slatkiše. Za godinu dana je smršao oko 30kg. Hidrogenizovane biljne masti u ,,eurokremu” oblažu ćelijske zidove kao izolacija, te hranljive materije ostaju bez efekta. Šećer menja naelektrisanje krvi, koje mora biti isto kao naelektrisanje kapilara, kako bi kapilari odbacivali krv i time potpomagali rad srca. Sa promenjenim naelektrisanjem, krv je privučena unutrašnjoj površini kapilara i time otežava rad srca; uz to ostavlja naslage i sužava prolaz. Ugljen-dioksid napada srce; kofein iz koka-kole povećava nivo mokraćne kiseline u krvi – nastupio je i giht, još jedna prepreka pešačenju, a on ga je primenjivao od svoje četvrte godine, samoinicijativno… Dalje je njegovo zdravstveno stanje oscilovalo u zavisnosti od samodiscipline. Februara 1999. godine onesvestio se na ulici, u oktobru je imao ponovo epistaksu, mnogo je iskrvario, zbog čega je pao u krevet, pa sam pozvala sveštenike da mu urade miropomazanje za bolesne. Posle toga sam pronašla da su vernici njegove, Hrišćanske adventističke crkve (u kojoj je, kao odrastao, ponovo kršten) dugovečniji od proseka, a među njima posebno oni koji svakog dana uzimaju jezgrasto voće. Uz to je počeo redovnije da jede grejpfrut, u čijoj se unutrašnjoj kori nalazi vitamin P, prepreka srčanoj i moždanoj kapi, održavanjem elastičnosti kapilarnih zidova. Od svoje desete godine jeo je i jabuke sa semenkama, gde ima digitalisa. Nesagledivu zaslugu u njegovom oporavku imao je i integralni pirinač. Nažalost, nekako smo propustili da uvrstimo gljive u redovnu ishranu, a to su najkvalitetnije belančevine, prvorazredna hrana po Bibliji. Preminuo je 2013, u svojoj pedesetoj godini. Ipak, poživeo je 14 godina posle miropomazanja.
On nije uzimao lekove kad je osetio da mu škode, ali ni njegovi lekari nisu ga podsticali u tome. U svakom slučaju, molitva, poslušnost Božjoj volji, u svemu pa i u ishrani po Svetom pismu, i to biljnom hranom, za koju danas imamo mogućnosti kao da smo u raju – pomogla bi svakome, i uz lekove i bez njih.