In an aesthetically decorated US government building, in a room hastily turned into a general staff, officers in elegant uniforms gather around a U-shaped table, running their eyes across the giant screen. The slides in PowerPoint for them show the last moves of the enemy who has now set an ambush in Saudi Arabia: this enemy is a mysterious virus responsible for the death of more than half of the people it has infected.
Here at the Centers for Disease Control and Prevention, uniformed experts from the US Public Health Service and their plainclothes colleagues have been meeting twice a week since early June to discuss the progress of the Middle East Respiratory Syndrome (MERS virus). MERS-CoV, as the microbe of such concern is called, causes a fever, severe cough, progressive renal failure and attacks the victim’s lungs.
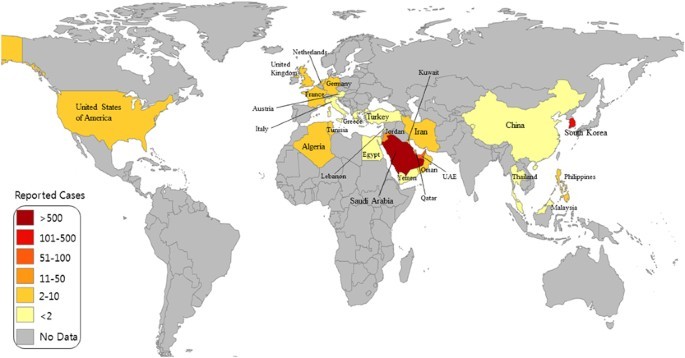
Since the coronavirus was first isolated in June 2012 in the city of Jeddah, at least 77 people have become infected with MERS, 40 of whom have died. The number of confirmed cases of the disease has quadrupled since April this year, with Turkish and British nationals among those affected. Most disturbing for healthcare professionals are the reports of patients who have not traveled in the Middle East. The virus has not yet appeared in the United States, but the future is uncertain.
Are you using your pain medication correctly? Check!
Especially that this month begins the pilgrimage season and probably 11 thousand. American Muslims will go to the Arabian Peninsula. In the meantime, millions of people will move between the continents of our globalized world. “A resident of New York can go to Saudi Arabia on business and bring the virus home,” notes Matthew Frieman, a virologist at the University of Maryland School of Medicine in Baltimore. There is no reason the virus should remain in the Middle East.
Many of the researchers who are trying to decode MERS today are among the veterans of the 2003 war with SARS, acute respiratory distress syndrome. A previously unknown coronavirus – a spherical, corona-shaped virus with protein projections – spread to people from bats and quickly began killing people in China and Hong Kong.
By the end of June 2003, more than 8400 people worldwide had contracted SARS, which was spreading rapidly in hospitals. US citizens emerged from the outbreak unscathed, but WHO warned against traveling to Toronto, where 16 deaths were recorded. The wave of diseases ended within a year thanks to effective preventive practices, such as wearing masks, quick diagnosis of patients and efficient first aid. The WHO said SARS caused 800 deaths worldwide and depleted local economies by $ 30 billion.
Scientists did not even think that coronaviruses, mainly responsible for colds and stomach flu, could be so dangerous. Therefore, the death of the first patient in Jeddah caused great consternation in the medical world. “We’ve since warned that there could be another tragic epidemic like SARS,” Frieman notes.
Research teams from around the world are trying to sequence the genetic code of a dangerous microbe. They’ve already determined that MERS must have appeared around 2011. Other researchers focused on mapping the MERS victims. First, they reported isolated cases in Saudi Arabia and Jordan, then in England, France and Italy, where sick patients from the Middle East sought medical attention. Most of the victims were male, many of whom had a history of heart disease and diabetes, further worsening their prognosis.
Epidemiologists began to observe clusters of disease forming when entire families or groups in the hospital became infected with MERS: people who were in close contact with those who were infected became infected. This has led scholars to fear that the virus has evolved into a new human-to-human form, a precondition for a pandemic.
One such case was reported in May of this year in the medical journal Lancet. In mid-April, a 64-year-old diabetic man with a kidney transplant in 1998 fell ill. Five days after traveling from Dubai to France, the patient felt sick, began to cough and complain of respiratory problems. He was admitted to the hospital in Valenciennes, where he found himself in the same room with a 51-year-old with a thrombosis in his arm. Three days later, the elderly patient was admitted to the intensive care unit, where his respiratory problems worsened, and the patient was diagnosed with kidney failure. It wasn’t until May 1 that doctors began to suspect MERS on him, and these fears were confirmed a week later. The man died of multiple organ failure.
Meanwhile, on April 30, the younger patient was discharged from the hospital, and about a week later began to complain of respiratory problems. The man had a long history of heart disease and, in a hospital room, his bed was less than a meter from the bed of an MERS patient. The patient was quickly transferred to the intensive care unit, where analyzes showed that he suffers from the same deadly coronavirus. He started to have a high fever, and his lungs and kidneys refused to obey him. He spent several weeks attached to life-saving equipment, and on May 29, while the report was being prepared on him, the patient was still alive.
Before the end of May this year, public health specialists located an exceptionally large concentration of 26 patients in Saudi Arabia’s Al-Ahsa region. In addition, smaller outbreaks of the disease were found in Great Britain, Italy and Tunisia.
The recorded increase in incidence could signal an increase in infection, although it is also likely that healthcare professionals are now diagnosing new cases more quickly and reporting them more frequently, says Ian Lipkin, an epidemiologist at Columbia University in New York. “We can’t tell,” he admits. – The increased number of cases may be a new fact or fact that we were not aware of before.
Many details about MERS remain a mystery to scholars. For example, researchers suspect that MERS, like SARS, originated in bats, but this hypothesis could not be confirmed. There is also a lack of data on whether it had spread to pets and livestock before the coronavirus started wreaking havoc among humans, notes Christian Drosten, of the Bonn Institute of Virology.
Meanwhile, scientists keep refining their methods of diagnosing sick people. Nasal and throat swab does not provide such unambiguous information about the patient’s health as the material taken directly from the lungs. Researchers cannot determine how many people have contracted MERS, but have not developed the symptoms characteristic of this syndrome. There is also a need to better understand how previous health problems of people with MERS influenced the incidence of coronavirus. Knowledge of this would “make a decisive impact” on further laboratory research, says Frieman.
Meanwhile, public health specialists went into the field. The World Health Organization wants to investigate the very source of the infection. In June, WHO officials traveled to Saudi Arabia to see how the kingdom is dealing with MERS, what efforts it is making to diagnose sick people quickly and prevent the spread of disease in hospitals. Saudi Arabia has reduced the number of visas issued to pilgrims this year. (…)
So far in the United States the alarm bell has rung 40 times, but none of the patients suspected of having MERS have had the disease. But even if a serious infection does not reach the US, US researchers have a keen interest in developing the epidemic – as well as developing methods to combat it at the international level – believing it to be a valuable investment for the future. Because in some time another microbe that is dangerous for people will undoubtedly appear. “This type of spreading infection is sure to repeat itself again,” Frieman warns.
Tekst: Eryn Brown