Contents
Lip commissure
A fragile and highly exposed area of the face, the corners of the lips can become the site of minor irritations, dryness, wounds or even an infection called angular cheilitis. All are generally benign but unsightly and sometimes painful in this very mobile area that is the mouth.
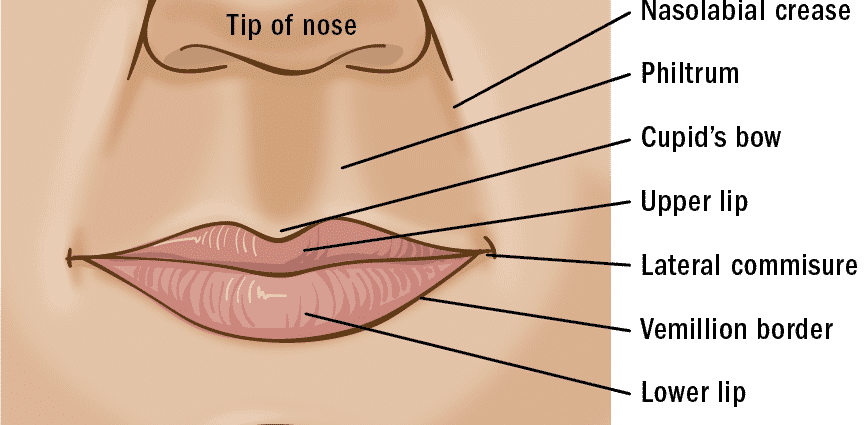
Anatomy
The corner of the lips refers to this fold on either side of the mouth, at the junction of the upper lip and the lower lip.
The problems of the corners of the lips
A drought
Exposed to the cold, to the wind, the corners of the lips can, like the lips for that matter, dry out quickly. The corners will then be red, and will tend to crack.
The perlèche
Like all intetrigos, that is to say the folded areas of the body, the corner of the lips is a favorable site for infections, especially mycotic, especially since it is often wet with saliva.
It happens that one or both corners of the lips is colonized by fungi or bacteria, causing symptoms that are as unsightly as they are painful. At the corners of the lips, the skin begins to take on a red and shiny appearance, then ends up cracking. Small sores tend to reopen regularly, bleed and then scab over due to frequent mouth movements.
The germs most often incriminated in this pathology called perléche or angular cheilitis of its scientific name are the fungus candida albicans (we will then speak of candidal perlèche) and staphylococcus aureus (bacterial perlèche). In the case of candidal perlèche, there is generally a whitish coating on the corner of the lips but also on the inside of the mouth and the tongue, often also affected by candidiasis. The presence of yellowish crusts leans more towards a perlèche due to a golden staphylococcus, which finds its reservoir in the nose. It can also be a bacterial superinfection of candidiasis. Much more rarely, angular cheilitis can be caused by the herpes or syphilis virus.
The infection is usually localized at the corner of the lips, but in people who are immunocompromised or frail, it can spread to the cheeks or inside the mouth.
Different factors favor the appearance of angular cheilitis: a dry mouth, the fact of licking the lips frequently, a small cut at the corner of the lips (during dental care or exposure to the cold for example) which will become a gateway for germs, ill-fitting dentures, diabetes, certain drugs (antibiotics, corticosteroids, immunosuppressants, retinoids), age which accentuates the folds of the corner of the lips, certain nutritional deficiencies (omega 3, vitamins group B, vitamin A, vitamin D, zinc).
Treatment
Drought treatment
Special moisturizers for lips or chapped skin can be applied to promote healing and help restore the skin’s hydro-lipid barrier. These are usually creams based on paraffin or mineral oils. They can be used daily for prevention as well.
Certain natural products are also recognized to promote the healing process:
- calendula oily macerate is renowned for its healing and antiseptic properties, perfect for damaged and irritated skin. Apply a few drops twice a day to the corners of irritated or cracked lips;
- honey can also be used on this fragile area for its antimicrobial, anti-inflammatory and healing properties. Preferably opt for a thyme or lavender honey, to be applied in a layer of one millimeter on the irritated area;
- shea butter can be used daily to hydrate the skin well and thus prevent chapping of the corners of the lips;
- aloe vera gel is also recognized for its moisturizing and healing properties.
Treatment of angular cheilitis
- In case of bacterial angular cheilitis, local antibiotic treatment based on fucidic acid may be prescribed. It must be accompanied by daily cleaning of the area with soap and water or, in case of superinfection, a local antiseptic (chlorhexidine or povidone iodine for example).
In the event of candidal perlèche, an antifungal cream will be prescribed. In case of signs of oral candidiasis, it will be associated with oral and local antifungal treatment of the mouth.
Diagnostic
A physical examination is sufficient to diagnose perleche. The presence of honey-colored scabs usually indicates Staphylococcus aureus. If in doubt, a sample can be taken to determine the origin of the infection.