Contents
Idiopathic fibrosing alveolitis (IFA) is a disease that remains one of the least studied, among other pathologies of the interstitium of the lungs. With this type of alveolitis, inflammation of the pulmonary interstitium occurs with its fibrosis. Suffer, including airways, lung parenchyma. This negatively affects the state of the respiratory organs, leads to their restrictive changes, disruption of gas exchange and respiratory failure, which causes death.
Idiopathic fibrosing alveolitis is also called idiopathic pulmonary fibrosis. This terminology is used mainly by English specialists (idiopathic pulmonary fibrosis), as well as German pulmonologists (idiopa-thische Lungenfibrose). In the UK, ELISA is called “cryptogenic fibrosing alveolitis” (cryptogenic fibrosing alveolitis).
The terms “cryptogenic” and “idiopathic” have some differences, but are now used interchangeably. Both of these words mean that the cause of the disease remains unclear.
Epidemiology and risk factors
Statistical information reflecting the prevalence of the disease is very contradictory. It is assumed that such discrepancies are due to the inclusion of patients not only with idiopathic fibrosing alveolitis, but also with other idiopathic interstitial pneumonias (IIP).
Out of 100 men, 000 people experience pathology, and 20 people out of 100 women. In a year, 000 people fall ill for every 13 men, and 100 people for every 000 women.
Although the causes of idiopathic alveolitis are currently unknown, scientists do not stop trying to find out the true nature of the origin of the disease. There is an assumption that the pathology has a genetic basis, when a person has a hereditary predisposition to the formation of fibrous tissues in the lungs. This happens in response to any damage to the cells of the respiratory system. Scientists confirm this hypothesis with a family history, when this disease is traced in blood relatives. Also in favor of the genetic basis of the disease is the fact that pulmonary fibrosis often manifests itself in patients with hereditary pathologies, for example, with Gaucher’s disease.
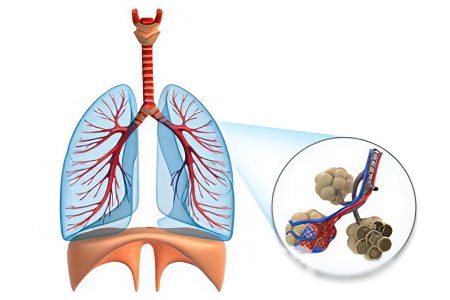
Structural changes in the lungs

The main characteristics of the morphological picture of idiopathic fibrosing alveolitis are:
The presence of dense fibrosis of the pulmonary parenchyma.
Morphological changes are distributed according to a patchy heterogeneous type. Such spotting is due to the fact that areas of healthy and damaged tissues alternate in the lungs. Changes can be fibrous, cystic, and in the form of interstitial inflammation.
The upper part of the acinus is included early in the inflammatory process.
In general, the histology of lung tissue in idiopathic fibrosing alveolitis resembles a similar picture as in interstitial pneumonia.
Symptoms of idiopathic fibrosing alveolitis

Most often, fibrosing idiopathic alveolitis is diagnosed in patients older than 50 years. Men get sick more often than women. The approximate ratio is 1,7:1.
Patients indicate shortness of breath, which is constantly increasing. The patient is unable to take a deep breath (inspiratory dyspnea), he is haunted by a dry cough without sputum. Dyspnea occurs in all patients with idiopathic fibrosing alveolitis.
The stronger the shortness of breath, the more severe the course of the disease. Having appeared once, it no longer passes, but only progresses. Moreover, its occurrence does not depend on the time of day, on the ambient temperature and other factors. The inspiratory phases in patients are shortened, as well as the expiratory phases. Therefore, the breathing of such patients is rapid. Each of them has hyperventilation syndrome.
If a person wants to take a deep breath, then this leads to a cough. However, not all patients develop a cough, so it is not of diagnostic interest. While in people with chronic obstructive pulmonary disease, which is often confused with ELISA, cough will always be present. As the disease progresses, shortness of breath leads to the fact that a person becomes disabled. He loses the ability to pronounce a long phrase, cannot walk and take care of himself on his own.
The manifesto of pathology is hardly noticeable. Some patients note that fibrosing alveolitis began to develop in them according to the type of SARS. Therefore, some scientists suggest that the disease may be of a viral nature. Since the pathology develops slowly, the person has time to adapt to his shortness of breath. Unbeknownst to themselves, people reduce their activity and move on to a more passive life.
A productive cough, that is, a cough that is accompanied by sputum production, develops in no more than 20% of patients. The mucus may contain pus, especially in those patients who suffer from severe idiopathic fibrosing alveolitis. This sign is dangerous, as it indicates the addition of a bacterial infection.
An increase in body temperature and the appearance of blood in the sputum are not typical for this disease. While listening to the lungs, the doctor auscultates the crepitus that occurs at the end of inspiration. If blood appears in the sputum, the patient should be referred for examination for lung cancer. This disease in patients with ELISA is diagnosed 4-12 times more often than in healthy people, even those who smoke.
Other symptoms of ELISA include:
Joint pain.
Muscle aches.
Deformities of the nail phalanges that begin to resemble drumsticks. This symptom occurs in 70% of patients.
Crepitations at the end of inhalation become more intense, and at the beginning they will be more gentle. Experts compare the final crepitus to the crackling of cellophane or the sound that is made when a zipper is opened.
If at an early stage of the development of the disease, crepitations are heard mainly in the posterior basal regions, then as it progresses, creaks will be heard over the entire surface of the lungs. Not at the end of the breath, but throughout its entire length. When the disease has just begun to develop, crepitus may be absent when the torso is tilted forward.
Dry rales are heard in no more than 10% of patients. The most common cause is bronchitis. Further development of the disease leads to symptoms of respiratory failure, the development of cor pulmonale. The color of the skin acquires an ash-cyanotic color, the 2nd tone over the pulmonary artery intensifies, the heartbeat quickens, the cervical veins swell, the limbs swell. The final stage of the disease leads to a pronounced weight loss of a person, up to the development of cachexia.
Diagnosis of idiopathic fibrosing alveolitis

Methods for diagnosing idiopathic fibrosing alveolitis at this point in time have been revised. Although such a research technique as an open lung biopsy gives the most reliable result and is considered the “gold standard” of diagnostics, it is not always practiced.
This is due to the significant disadvantages of an open lung biopsy, including: the procedure is invasive, it is expensive, after its implementation, treatment will need to be postponed until the patient recovers. In addition, it will not be possible to perform a biopsy several times. It is completely impossible for a certain part of patients to perform it, since the state of human health does not allow it.
The basic diagnostic criteria that have been developed to detect idiopathic fibrosing alveolitis are:
Other pathologies of the interstitium of the lungs are excluded. This refers to diseases that could be triggered by taking medications, inhaling harmful substances, systemic damage to the connective tissue.
The function of external respiration is reduced, gas exchange in the lungs is disturbed.
During the CT scan, bilateral mesh changes are detected in the lungs, in their basal sections.
Other diseases are not confirmed after transbronchial biopsy or bronchoalveolar lavage.
Additional diagnostic criteria include:
The patient is over 50 years old.
Shortness of breath occurs imperceptibly for the patient, increases with physical exertion.
The disease has a long course (from 3 months or more).
Crepitus is heard in the basal regions of the lungs.
In order for the doctor to be able to make a diagnosis, it is necessary to find confirmation of 4 main criteria and 3 additional ones. Evaluation of clinical criteria makes it possible to determine ELISA with a high degree of probability, up to 97% (data provided by Raghu et al.), but the sensitivity of the criteria itself is equal to 62%. Therefore, about a third of patients still need to perform a lung biopsy.
High-precision computed tomography improves the quality of lung examination and facilitates the diagnosis of ELISA, as well as other similar pathologies. Its research value is equal to 90%. Many experts insist on completely abandoning the biopsy, provided that high-precision tomography has revealed changes characteristic of idiopathic alveolitis. In this case, we are talking about a “honeycomb” lung (when the affected area is 25%), as well as histological confirmation of the presence of fibrosis.
Laboratory diagnostics has no global significance in terms of pathology detection.
The main characteristics of the obtained analyzes:
Moderate increase in ESR (diagnosed in 90% of patients). If the ESR increases significantly, then this may indicate a cancerous tumor, or an acute infection.
Increased cryoglobulins and immunoglobulins (in 30-40% of patients).
An increase in antinuclear and rheumatoid factors, but without revealing systemic pathology (in 20-30% of patients).
An increase in the serum level of total lactate dehydrogenase, which is due to the increased activity of alveolar macrophages and type 2 alveocytes.
Increased hematocrit and red blood cells.
An increase in the level of leukocytes. This indicator may be a sign of an infection, or a sign of taking glucocorticosteroids.
Since fibrosing alveolitis leads to disturbances in the functioning of the lungs, it is important to evaluate their volume, that is, their vital capacity, total capacity, residual volume and functional residual capacity. When performing the test, the Tiffno coefficient will be within the normal range, or even increase. Analysis of the pressure-volume curve will show its shift to the right and down. This indicates a decrease in the extensibility of the lungs and a decrease in their volume.
The described test is highly sensitive, so it can be used for early diagnosis of pathology, when other studies do not yet detect any changes. For example, a blood gas test performed at rest will not reveal any abnormalities. A decrease in the partial tension of oxygen in arterial blood is observed only during physical exertion.
In the future, hypoxemia will be present even at rest and be accompanied by hypocapnia. Hypercapnia develops only at the final stage of the disease.
When conducting radiography, it is most often possible to visualize changes of the reticular or reticulonodular type. They will be found in both lungs, in their lower part.
Reticular tissue with fibrosing alveolitis becomes rough, strands are formed in it, cystic enlightenments with a diameter of 0,5-2 cm. They form the picture of a “honeycomb lung”. When the disease reaches the terminal stage, it is possible to visualize the deviation of the trachea to the right and tracheomegaly. At the same time, specialists should take into account that in 16% of patients, the x-ray picture may remain within the normal range.
If the pleura is involved in the pathological process in a patient, intrathoracic adenopathy develops and parenchymal thickening becomes noticeable, then this may indicate a complication of ELISA by a cancerous tumor, or another lung disease. If a patient simultaneously develops alveolitis and emphysema, then the lung volume may remain within the normal range, or even be increased. Another diagnostic sign of the combination of these two diseases is the weakening of the vascular pattern in the upper part of the lungs.

During high-resolution computed tomography, doctors detect the following signs:
Irregular linear shadows.
Cystic lucidity.
Focal foci of reduced transparency of the lung fields of the “frosted glass” type. The area of damage to the lungs is 30%, but no more.
Thickening of the walls of the bronchi and their irregularity.
Disorganization of the lung parenchyma, traction bronchiectasis. The basal and subpleural regions of the lungs are most affected.
If the CT data is evaluated by a specialist, then the diagnosis will be 90% correct.
This study makes it possible to distinguish between idiopathic fibrosing alveolitis and other diseases that have a similar picture, including:
Chronic hypersensitivity pneumonitis. With this disease, the patient does not have “cellular” changes in the lungs, centrilobular nodules are noticeable, and the inflammation itself is concentrated in the upper and middle parts of the lungs.
Asbestosis. In this case, the patient develops pleural plaques and parenchymal bands of fibrosis.
Desquamative interstitial pneumonia. Blackouts of the “frosted glass” type will be extended.
According to computed tomography, it is possible to make a prognosis for the patient. It will be better for patients with ground glass syndrome, and worse for patients with reticular changes. An intermediate prognosis is indicated for patients with mixed symptoms.
This is due to the fact that patients with ground glass syndrome respond better to glucocorticosteroid therapy, which is reflected by characteristic signs during HRCT. Now doctors are more guided by computed tomography data when making a prognosis than by other methods (bronchial and alveolar lavage, lung tests, lung biopsy). It is computed tomography that makes it possible to assess the degree of involvement of the lung parenchyma in the pathological process. While a biopsy makes it possible to examine only a certain part of the body.
Bronchoalveolar lavage should not be excluded from diagnostic practice, as it makes it possible to determine the prognosis of the pathology, its course and the presence of inflammation. In lavage with ELISA, an increased number of eosinophils and neutrophils is found. At the same time, this symptom is characteristic of other diseases of the lung tissue, so its significance should not be overestimated.
A high level of eosinophils in lavage worsens the prognosis of idiopathic fibrosing alveolitis. The fact is that such patients most often respond poorly to treatment with corticosteroid drugs. Their use allows to reduce the level of neutrophils, but the number of eosinophils remains the same.
If high concentrations of lymphocytes are found in the lavage fluid, this may indicate a favorable prognosis. Since their increase often occurs with an adequate response of the body to treatment with corticosteroids.
Transbronchial biopsy allows you to get only a small area of tissue (no more than 5 mm). Therefore, the informative value of the study is reduced. Since this method is relatively safe for the patient, it is practiced in the early stages of the disease. A biopsy can exclude pathologies such as sarcoidosis, hypersensitivity pneumonitis, cancerous tumors, infections, eosinophilic pneumonia, histocytosis, and alveolar proteinosis.
As mentioned, an open-type biopsy is considered a classic method for diagnosing ELISA, it allows you to accurately diagnose, but it is impossible to predict the development of pathology and its response to future treatment using this method. An open biopsy can be replaced by a thoracoscopic biopsy.
This study involves taking a similar amount of tissue, but the duration of the drainage of the pleural cavity is not so long. This reduces the time the patient spends in the hospital. Complications from a thoracoscopic procedure are less common. As studies show, an open biopsy is not advisable to prescribe to all patients without exception. It is really required only by 11-12% of patients, but no more.
In the international classification of diseases of the 10th revision, ELISA is defined as “J 84.9 – Interstitial pulmonary disease, unspecified.”
The diagnosis can be formulated as follows:
ELISA, early stage, respiratory failure of the 1st degree.
ELISA at the stage of “cellular lung”, respiratory failure of the 3rd degree, chronic cor pulmonale.
Treatment of idiopathic fibrosing alveolitis
Effective methods for the treatment of ELISA have not yet been developed. Moreover, it is difficult to give a conclusion about the effectiveness of the results of therapy, since data on the natural course of the disease are minimal.
Treatment is based on the use of drugs that reduce the inflammatory response. Corticosteroids and cytostatics are used, which affect the human immune system and help reduce inflammation. Such therapy is explained by the assumption that idiopathic fibrosing alveolitis develops against a background of chronic inflammation, which entails fibrosis. If this reaction is suppressed, then the formation of fibrotic changes can be prevented.
There are three possible avenues of therapy:
Treatment with glucocorticosteroids only.
Treatment with glucocorticosteroids with azathioprine.
Treatment with glucocorticosteroids with cyclophosphamide.
The international consensus, held in 2000, advises the use of the last 2 regimens in the treatment, although there are no arguments in favor of their effectiveness compared with glucocorticosteroid monotherapy.
Many doctors today prescribe glucocorticosteroids for oral administration. While it is possible to achieve positive results only in 15-20% of patients. Persons younger than 50 years of age, mostly women, respond better to such therapy if they have increased values of lymphocytes in the lavage from the bronchi and alveoli, and ground glass changes are also diagnosed.
Treatment should continue for at least six months. To evaluate its effectiveness, pay attention to the symptoms of the disease, the results of x-rays and other techniques. During treatment, it is necessary to monitor the patient’s well-being, since such therapy is associated with a high risk of complications.
There are some experts who oppose the use of cytostatics in the treatment of ELISA. They justify this by saying that the likelihood of complications with such therapy is extremely high. This is especially true in the case of the use of Cyclophosphamide. The most common side effect is pancytopenia. If the platelets fall below 100/ml, or the level of lymphocytes falls below 000/ml, then the dosage of the drugs is reduced.
In addition to leukopenia, treatment with cyclophosphamide is associated with the development of such side effects as:
Bladder cancer.
Hemorrhagic cystitis.
Stomatitis.
Chair disorder.
High susceptibility of the body to infectious diseases.
If the patient was nevertheless prescribed cytostatics, then every week he will have to donate blood for a general analysis (during the first 30 days from the start of treatment). Then blood is given 1-2 times in 14-28 days. If therapy is carried out using Cyclophosphamide, then every week the patient should bring urine for analysis. It is important to assess her condition and control the appearance of blood in the urine. Such control in home treatment can be difficult to implement, therefore, such a therapy regimen is not always used.
Scientists hope that the use of interferons will help to cope with idiopathic fibrosing alveolitis. They prevent the germination of fibroblasts and matrix protein in the cells of the lung tissue.
A radical way to treat pathology is lung transplantation. Survival of patients within 3 years after surgery is 60%. However, many patients with ELISA are elderly, so they cannot tolerate such an intervention.
Treatment of complications
If the patient develops a respiratory infection, then he is prescribed antibiotics and antimycotics. Doctors insist that such patients be vaccinated against influenza and pneumococcal infection. Therapy of pulmonary hypertension and decompensated chronic cor pulmonale is carried out according to the relevant protocols.
If the patient manifests hypoxemia, then he is shown oxygen therapy. This makes it possible to reduce shortness of breath and increase the patient’s exercise tolerance.
Forecast
The prognosis in patients with idiopathic fibrosing alveolitis is poor. The average life expectancy of such patients does not exceed 2,9 years.
The prognosis is somewhat better in sick women, in young patients, but only on condition that the disease lasts no more than a year. It also improves the prognosis of a positive response of the body to treatment with glucocorticosteroids.
Most often, patients die from respiratory and pulmonary heart failure. These complications develop due to the progression of ELISA. It can also be fatal due to lung cancer.









