Contents
Exogenous allergic alveolitis is also called hypersensitivity pneumonitis. The abbreviation for the disease is EAA. This term reflects a whole group of diseases that affect the interstitium of the lungs, that is, the connective tissue of organs. Inflammation is concentrated in the lung parenchyma and small airways. It occurs when a variety of antigens (fungi, bacteria, animal proteins, chemicals) enter them from the outside.
For the first time, exogenous allergic alveolitis was described by J.
In the future, it was possible to establish that allergic alveolitis of the exogenous type can be triggered by other causes. In particular, in 1965, C. Reed and his colleagues found similar symptoms in three patients who were breeding pigeons. They began to call such an alveolitis “the lung of bird lovers.”
The statistics of recent years indicate that the disease is quite widespread among people who, due to their professional activities, interact with feathers and down of birds, as well as with compound feed. Out of 100 population, exogenous allergic alveolitis will be diagnosed in 000 people. At the same time, it is impossible to accurately predict which particular person who is allergic to down or feathers will develop alveolitis.
As practice shows, from 5 to 15% of people who interacted with high concentrations of allergens will develop pneumonitis. The prevalence of alveolitis among individuals who work with low concentrations of sensitizing substances is not known to date. However, this problem is quite acute, as the industry develops more and more intensively every year, which means that more and more people are involved in such activities.
Etiology
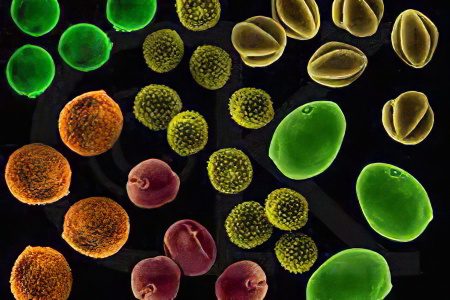
Allergic alveolitis develops due to the inhalation of an allergen, which enters the lungs along with the air. Various substances can act as an allergen. The most aggressive allergens in this regard are fungal spores from rotten hay, maple bark, sugar cane, etc.
Also, one should not write off plant pollen, protein compounds, house dust. Some medicines, such as antibiotics or nitrofuran derivatives, can cause allergic alveolitis even without previous inhalation, and after entering the body in other ways.
Not only the fact that allergens enter the respiratory tract is important, but also their concentration and size. If the particles do not exceed 5 microns, then it will not be difficult for them to reach the alveoli and provoke a hypersensitivity reaction in them.
Since allergens that cause EAA are most often associated with a person’s professional activities, varieties of alveolitis were named for various professions:
Farmer’s Lung. Antigens are found in moldy hay, among them: Thermophilic Actinomycetes, Aspergillus spp, Mycropolyspora faeni, Thermoactinomycas vulgaris.
The lung of bird lovers. Allergens are found in the excrement and dander of birds. They become whey proteins of birds.
Bagassoz. The allergen is sugar cane, namely Mycropolysporal faeni and Thermoactinomycas sacchari.
The lung of persons growing mushrooms. Compost becomes the source of allergens, and Mycropolysporal faeni and Thermoactinomycas vulgaris act as antigens.
Lung of persons using conditioners. Humidifiers, heaters, and air conditioners are sources of antigens. Sensitization is provoked by such pathogens as: Thermoactinomycas vulgaris, Thermoactinomycas viridis, Ameba, Fungi.
Suberose. The bark of the cork tree becomes the source of allergens, and Penicillum frequentans acts as the allergen itself.
Light malt brewers. The source of antigens is moldy barley, and the allergen itself is Aspergillus clavatus.
Cheesemaker’s disease. The source of antigens is cheese and mold particles, and the antigen itself is Penicillum cseii.
Sequoyz. Allergens are found in redwood wood dust. They are represented by Graphium spp., upullaria spp., Alternaria spp.
Lung detergent manufacturers. The allergen is found in enzymes and detergents. It is represented by Bacillus subtitus.
Lung laboratory workers. The sources of allergens are dandruff and rodent urine, and the allergens themselves are represented by the proteins of their urine.
Lung sniffing pituitary powder. The antigen is represented by porcine and bovine proteins, which are found in the powder of the pituitary gland.
Lung employed in the production of plastics. The source leading to sensitization is diisocyanates. The allergens are: Toluene diiosocianate, diphenylmethane diiosocianate.
Summer pneumonitis. The disease develops due to the inhalation of dust from damp living quarters. The pathology is widespread in Japan. Trichosporon cutaneum becomes a source of allergens.

Of the listed allergens in terms of the development of exogenous allergic alveolitis, thermophilic actinomycetes and bird antigens are of particular importance. In areas with a high development of agriculture, it is actinomycetes that occupy a leading position in terms of the incidence of EAA. They are represented by bacteria that do not exceed a size of 1 micron. A distinctive feature of such microorganisms is that they have the properties of not only microbes, but also fungi. Many thermophilic actinomycetes are located in the soil, in compost, in water. They also live in air conditioners.
Such types of thermophilic actinomycetes lead to the development of exogenous allergic alveolitis, such as: Mycropolyspora faeni, Thermoactinomycas vulgaris, Thermoactinomycas viridis, Thermoactinomycas sacchari, Thermoactinomycas scandidum.
All of the listed representatives of flora pathogenic for humans begin to multiply actively at a temperature of 50-60 °C. It is under such conditions that the processes of decay of organic matter are launched. A similar temperature is maintained in heating systems. Actinomycetes can cause bagassosis (lung disease in people who work with sugarcane), cause a disease called “farmer’s lung”, “lung of mushroom pickers (mushroom growers)”, etc. All of them are listed above.
The antigens that affect humans interacting with birds are serum proteins. These are albumin and gamma globulins. They are present in bird droppings, in secretions from the skin glands of pigeons, parrots, canaries, etc.
People who care for birds experience alveolitis with prolonged and regular interaction with animals. Proteins of cattle, as well as pigs, are capable of provoking the disease.
The most active fungal antigen is Aspergillus spp. Various species of this microorganism can cause suberosis, malt brewer’s lung or cheese maker’s lung.
It is in vain to believe that, living in the city and not doing agriculture, a person cannot get sick with exogenous allergic alveolitis. In fact, Aspergillus fumigatus thrives in damp areas that are rarely ventilated. If the temperature in them is high, then microorganisms begin to multiply rapidly.
Also at risk for the development of allergic alveolitis are people whose professional activities are associated with reactogenic chemical compounds, for example, plastic, resins, paints, polyurethane. Phthalic anhydride and diisocyanate are considered especially dangerous.
Depending on the country, the following prevalence of different types of allergic alveolitis can be traced:
The lung of budgerigar lovers is most often diagnosed in residents of the UK.
The lung of persons using air conditioners and humidifiers is in America.
The summer type of alveolitis, caused by the seasonal reproduction of fungi of the Trichosporon cutaneun species, is diagnosed in 75% of cases in the Japanese.
In Moscow and in cities with large industrial enterprises, patients with a reaction to bird and fungal antigens are most often detected.
Pathogenesis of exogenous allergic alveolitis
The human respiratory system regularly encounters dust particles. And this applies to both organic and inorganic contaminants. It has been established that antigens of the same type can cause the development of various pathologies. Some people develop bronchial asthma, others develop chronic rhinitis. There are also people who manifest allergic dermatosis, that is, skin lesions. We must not forget about conjunctivitis of an allergic nature. Naturally, exogenous alveolitis is not the last in the list of listed pathologies. What kind of disease a particular person will develop depends on the strength of the exposure, on the type of allergen, the state of the body’s immune system and other factors.
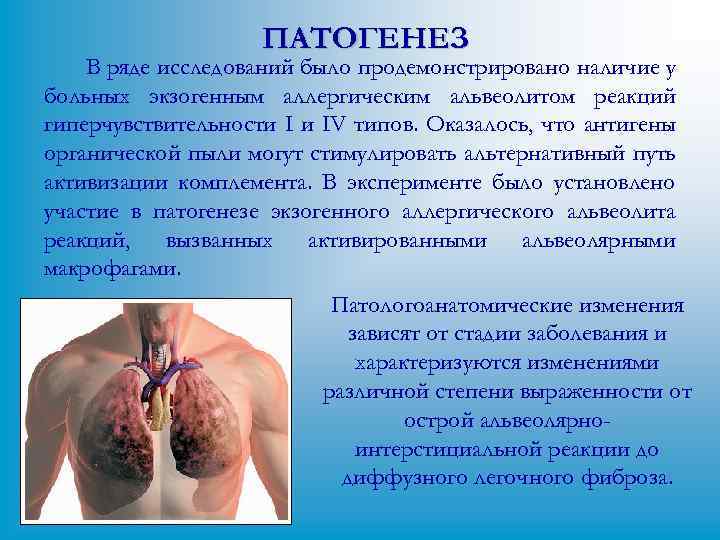
In order for a patient to manifest exogenous allergic alveolitis, a combination of several factors is necessary:
A sufficient dose of allergens that have entered the respiratory tract.
Prolonged exposure to the respiratory system.
A certain size of pathological particles, which is 5 microns. Less commonly, the disease develops when large antigens enter the respiratory system. In this case, they should settle in the proximal bronchi.
The vast majority of people who encounter such allergens do not suffer from EAA. Therefore, scientists believe that the human body should be affected simultaneously by several factors at once. They have not been studied enough, but there is an assumption that genetics and the state of immunity matter.
Exogenous allergic alveolitis is rightfully referred to as immunopathological diseases, the undoubted cause of which are allergic reactions of types 3 and 4. Also, non-immune inflammation should not be ignored.
The third type of immunological reaction is of particular importance in the initial stages of the development of pathology. The formation of immune complexes occurs directly in the interstitium of the lungs when a pathological antigen interacts with antibodies of the IgG class. The formation of immune complexes leads to the fact that the alveoli and interstitium is damaged, the permeability of the vessels that feed them increases.
The resulting immune complexes cause the complement system and alveolar macrophages to become activated. As a result, toxic and anti-inflammatory products, hydrolytic enzymes, cytokines (tumor necrosis factor – TNF-a and interleukin-1) are released. All this causes an inflammatory reaction at the local level.
Subsequently, the cells and matrix components of the interstitium begin to die, inflammation becomes more intense. Significant amounts of monocytes and lymphocytes are supplied to the site of the lesion. They ensure the preservation of the delayed-type hypersensitivity reaction.
Facts that confirm that immunocomplex reactions are important in exogenous allergic alveolitis:
After interaction with the antigen, inflammation develops rapidly, within 4-8 hours.
In washings of exudate from the bronchi and alveoli, as well as in the serum part of the blood, high concentrations of antibodies of the lgG class are found.
In the lung tissue taken for histology, in patients with an acute form of the disease, immunoglobulin, complement components, and the antigens themselves are found. All these substances are immune complexes.
When performing skin tests using highly purified antigens that are pathological for a particular patient, a classic Arthus-type reaction develops.
After performing provocative tests with the inhalation of pathogens, the number of neutrophils in patients in the bronchoalveolar lavage fluid increases.
Type 4 immune responses include CD+ T-cell delayed-type hypersensitivity and CD8+ T-cell cytotoxicity. After antigens enter the respiratory system, delayed-type reactions develop in 1-2 days. Damage to immune complexes leads to the release of cytokines. They, in turn, cause leukocytes and the endothelium of the lung tissue to express adhesive molecules on the surface. Monocytes and other lymphocytes react to them, which actively arrive at the site of the inflammatory reaction.
At the same time, interferon gamma activates macrophages that produce CD4 + lymphocytes. This is the hallmark of a delayed-type reaction, which lasts for a long time thanks to macrophages. As a result, granulomas form in the patient, collagen begins to be released in excess amounts (fibroblasts are activated by growth cells), and interstitial fibrosis develops.
Facts that confirm that in exogenous allergic alveolitis, delayed type 4 immunological reactions are important:
T-lymphocytes are found in the blood memory. They are present in the lung tissue of patients.
In patients with acute and subacute exogenous allergic alveolitis, granulomas, infiltrates with accumulation of lymphocytes and monocytes, as well as interstitial fibrosis are detected.
Experiments on laboratory animals with EAA have shown that CD4+ T-lymphocytes are required for disease induction.
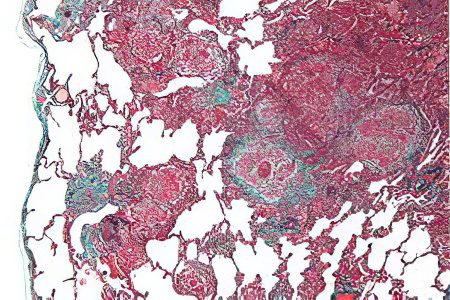
Histological picture of EAA
In most cases, patients with exogenous allergic alveolitis have granulomas, without curdled plaque. They are detected in 79-90% of patients.
In order not to confuse granulomas that develop with EAA and with sarcoidosis, you need to pay attention to the following differences:
With EAA, the granulomas are smaller.
Granulomas do not have clear boundaries.
Granulomas contain more lymphocytes.
Alveolar walls in EAA are thickened, they have lymphocytic infiltrates.
After contact with the antigen is excluded, the granulomas disappear on their own within six months.
In exogenous allergic alveolitis, the inflammatory process is caused by lymphocytes, monocytes, macrophages and plasma cells. Foamy alveolar macrophages accumulate inside the alveoli themselves, and lymphocytes in the interstitium. When the disease has just begun to develop, patients have a protein and fibrinous effusion, which is located inside the alveoli. Also, patients are diagnosed with bronchiolitis, lymphatic follicles, peribronchial inflammatory infiltrates, which are concentrated in the small airways.
So, the disease is characterized by a triad of morphological changes:
Alveolitis.
Granulomatosis.
Bronchiolitis.
Although sometimes one of the signs may fall out. Rarely, patients with exogenous allergic alveolitis develop vasculitis. He was diagnosed in a patient posthumously, as indicated in the relevant documents. In patients with pulmonary hypertension, hypertrophy of the arteries and arterioles occurs.
The chronic course of EAA leads to fibrinous changes, which can have different intensity. However, they are characteristic not only for exogenous allergic alveolitis, but also for other chronic lung diseases. Therefore, it cannot be called a pathognomic sign. With long-term alveolitis in patients, the lung parenchyma undergoes pathological changes in the type of honeycomb lung.
Symptoms of exogenous allergic alveolitis

The disease develops most often in people who are not prone to allergic reactions. Pathology manifests itself after prolonged interaction with sources, the spread of antigens.
Exogenous allergic alveolitis can occur in 3 types:
Acute symptoms
The acute form of the disease occurs after a large amount of antigen enters the respiratory tract. This can happen both at home and at work or even on the street.
After 4-12 hours, a person’s body temperature rises to high levels, chills develop, and weakness increases. There is heaviness in the chest, the patient begins to cough, he is haunted by shortness of breath. Aches appear in the joints and muscles. Sputum during coughing does not appear often. If it leaves, then it is small and it consists mainly of mucus.
Another symptom characteristic of acute EAA is a headache that focuses on the forehead.
During the examination, the doctor notes cyanosis of the skin. When listening to the lungs, crepitations and wheezing are heard.
After 1-3 days, the symptoms of the disease disappear, but after another interaction with the allergen, they increase again. General weakness and lethargy, combined with shortness of breath, can disturb a person for several weeks after the resolution of the acute stage of the disease.
The acute form of the disease is not often diagnosed. Therefore, doctors confuse it with SARS, provoked by viruses or mycoplasmas. Experts should be alert to farmers, and also distinguish between the symptoms of EAA and the symptoms of pulmonary mycotoxicosis, which develop when fungal spores enter the lung tissue. In patients with myotoxicosis, lung radiography does not show any pathological changes, and there are no precipitating antibodies in the serum part of the blood.
subacute symptoms
Symptoms of the subacute form of the disease are not as pronounced as in the acute form of alveolitis. Such an alveolitis develops due to prolonged inhalation of antigens. Most often this happens at home. So, subacute inflammation in most cases is provoked by the care of poultry.
The main manifestations of subacute exogenous allergic alveolitis include:
Shortness of breath that worsens after a person’s physical activity.
Increased fatigue.
Cough that produces clear sputum.
At an early stage in the development of pathology, body temperature may increase.
Crepitus when listening to the lungs will be gentle.
It is important to distinguish subacute EAA from sarcoidosis and other interstitium diseases.
Symptoms of the chronic type
The chronic form of the disease develops in people who interact with small doses of antigens for a long time. In addition, subacute alveolitis can become chronic if it is not treated.
The chronic course of the disease is indicated by symptoms such as:
Increasing over time, shortness of breath, which becomes apparent with physical exertion.
Pronounced weight loss, which can reach anorexia.
The disease threatens with the development of cor pulmonale, interstitial fibrosis, heart and respiratory failure. Since chronic exogenous allergic alveolitis begins to develop latently and does not give severe symptoms, its diagnosis is difficult.
Diagnosis of exogenous allergic alveolitis

To identify the disease, it is necessary to rely on an X-ray examination of the lungs. Depending on the stage of development of alveolitis and its form, radiological signs will differ.
The acute and subacute form of the disease leads to a decrease in the transparency of fields like ground glass and to the spread of nodular-mesh opacities. The size of the nodules does not exceed 3 mm. They can be found over the entire surface of the lungs.
The upper part of the lungs and their basal sections are not covered with nodules. If a person stops interacting with antigens, then after 1-1,5 months, the radiological signs of the disease disappear.
If the disease has a chronic course, then linear shadows with a clear outline, dark areas represented by nodules, changes in the interstitium, and a decrease in the size of the lung fields are visible on the x-ray picture. When the pathology has a running course, the honeycomb lung is visualized.
CT is a method that has a much higher accuracy compared to radiography. The study reveals signs of EAA, which are invisible with standard radiography.
A blood test in patients with EAA is characterized by the following changes:
Leukocytosis up to 12-15×103/ml Less commonly, the level of leukocytes reaches the level of 20-30×103/ ml.
The leukocyte formula shifts to the left.
An increase in the level of eosinophils does not occur, or it may increase slightly.
ESR in 31% of patients rises to 20 mm/h, and in 8% of patients up to 40 mm/h. In other patients, ESR remains within the normal range.
The level of lgM and lgG increases. Sometimes there is a jump in class A immunoglobulins.
In some patients, rheumatoid factor is activated.
Increases the level of total LDH. If this occurs, then acute inflammation in the lung parenchyma can be suspected.
To confirm the diagnosis, Ouchterlony double diffusion, micro-Ouchterlony, counter immunoelectrophoresis and ELISA (ELISA, ELIEDA) methods are used. They allow you to identify specific precipitating antibodies to the antigens that caused the allergy.
In the acute phase of the disease, precipitating antibodies will circulate in the blood of virtually every patient. When the allergen ceases to interact with the lung tissue of patients, the level of antibodies drops. However, they can be present in the serum part of the blood for a long time (up to 3 years).
When the disease is chronic, antibodies are not detected. There is also the possibility of false positive results. In farmers without symptoms of alveolitis, they are detected in 9-22% of cases, and in bird lovers in 51% of cases.
In patients with EAA, the value of precipitating antibodies does not correlate with the activity of the pathological process. Their level can be affected by a variety of factors. So, in smokers, it will be underestimated. Therefore, the detection of specific antibodies cannot be considered evidence of EAA. At the same time, their absence in the blood does not indicate that there is no disease. However, antibodies should not be written off, as in the presence of appropriate clinical signs, they can strengthen the existing assumption.
The test for a decrease in the diffuse capacity of the lungs is indicative, since other functional changes in EAA are characteristic of other types of pathologies accompanied by damage to the interstitium of the lungs. Hypoxemia in patients with allergic alveolitis is observed in a calm state, and increases during physical exertion. Violation of ventilation of the lungs occurs by a restrictive type. Signs of airway hyperreactivity are diagnosed in 10-25% of patients.
Inhalation tests were first used to detect allergic alveolitis as early as 1963. Aerosols were made from dust taken from moldy hay. They led to an exacerbation of the symptoms of the disease in patients. At the same time, extracts taken from “pure hay” did not cause such a reaction in patients. In healthy individuals, even aerosols with mold did not provoke pathological signs.
Provocative tests in patients with bronchial asthma do not cause the appearance of rapid immunological reactions, do not provoke disturbances in the functioning of the lungs. While in people with a positive immune response, they lead to changes in the functioning of the respiratory system, to an increase in body temperature, chills, weakness and dyspnea. After 10-12 hours, these manifestations disappear on their own.
It is possible to confirm the diagnosis of EAA without performing provocative tests, so they are not used in modern medical practice. They are used only by experts who need to confirm the cause of the disease. Alternatively, it is enough to observe the patient in his usual conditions, for example, at work or at home, where there is contact with the allergen.
Bronchoalveolar lavage (BAL) allows you to assess the composition of the contents of the alveoli and distant parts of the lungs. The diagnosis can be confirmed by the detection of a five-fold increase in cellular elements in it, and 80% of them will be represented by lymphocytes (mainly T-cells, namely CD8 + lymphocytes).
The immunoregulatory index in patients is reduced to less than one. With sarcoidosis, this figure is 4-5 units. However, if lavage was performed in the first 3 days after the acute development of alveolitis, then the number of neutrophils will be increased, and lymphocytosis is not observed.
In addition, lavage makes it possible to detect an increase in the number of mast cells tenfold. This concentration of mast cells can persist for up to 3 months or more after contact with the allergen. This indicator characterizes the activity of the fibrin production process. If the disease has a subacute course, then plasma cells will be found in the lavage.
Making a differential diagnosis

Diseases from which exogenous allergic alveolitis must be distinguished:
Alveolar cancer or lung metastases. With cancerous tumors, there is no connection between the symptoms of the disease that have appeared and contact with allergens. Pathology is constantly progressing, characterized by severe manifestations. In the serum part of the blood, precipitating antibodies to allergens are not released. Also, information can be clarified using x-ray of the lungs.
miliary tuberculosis. With this disease, there is also no relationship with allergens. The infection itself has a severe course and a long development. Serological techniques make it possible to detect antibodies to the tuberculosis antigen, while they do not appear to exoallergens. Do not forget about x-ray examination.
Sarcoidosis. This disease is not associated with the professional activity of a person. With it, not only the respiratory organs are affected, but also other body systems. The hilar lymph nodes in the chest become inflamed on both sides, there is a weak or negative reaction to tuberculin. Kveim’s reaction, on the contrary, will be positive. Sarcoidosis can be confirmed by histological examination.
Other fibrosing alveolitis. With them, most often, patients develop vasculitis, and systemic damage to the connective tissue concerns not only the lungs, but also the body as a whole. With a doubtful diagnosis, a lung biopsy is performed with further histological examination of the material obtained.
Pneumonia. This disease develops after a cold. On the x-ray, blackouts are visible, which appear due to tissue infiltration.
ICD-10 refers exogenous allergic alveolitis to class X “Respiratory diseases”.
Clarifications:
J 55 Respiratory disease caused by specific dust.
J 66.0 Byssinosis.
J 66.1 Disease of flax flayers.
J 66.2 Cannabiosis.
J 66.8 Respiratory disease due to other specified organic dusts.
J 67 Hypersensitivity pneumonitis.
J 67.0 Lung of a farmer (agricultural worker).
J 67.1 Bagassose (for sugar cane dust)
J 67.2 Poultry breeder’s lung.
J 67.3 Suberoz
J 67.4 Malt worker’s lung.
J 67.5 Mushroom worker’s lung.
J 67.6 Maple bark lung.
J 67.8 Hypersensitivity pneumonitis due to other organic dusts.
J 67.9 Hypersensitivity pneumonitis due to other unspecified organic dust.
The diagnosis can be formulated as follows:
Exogenous allergic alveolitis (farmer’s lung), acute form.
Drug-induced allergic alveolitis caused by furazolidone, subacute form, with respiratory failure.
Exogenous allergic alveolitis (poultry breeder’s lung), chronic form. Chronic lung heart, chronic bronchitis.
Treatment of exogenous allergic alveolitis
To cope with the disease, it is necessary to completely exclude the interaction of the patient and the allergen. A person during work must use masks, special filters. It is highly desirable to change jobs and your habits. In order to prevent the progression of pathology, it is important to identify it in the early stages of development. If contact with the allergen continues, the changes in the lungs will become irreversible.
The severe course of alveolitis requires the appointment of glucocorticosteroids. They can only be prescribed by a doctor, by appointment.
Patients with hyperresponsiveness of the lungs are prescribed inhaled bronchodilators. If the disease has led to the development of complications, then antibiotics, diuretics, oxygen, etc. are used.
Prognosis and prevention

To prevent the development of the disease, it is necessary to minimize all possible contact with allergens. So, hay should be thoroughly dried, silo pits should be open. Premises in production should be thoroughly ventilated, and if animals and birds are in them, sanitary and hygienic requirements should be strictly observed. Air conditioners and ventilation systems must be processed with high quality and on time, etc.
If the alveolitis has already developed, then the patient should exclude contact with allergens. When professional activity becomes the fault, the job is changed.
The prognosis varies. If the disease was diagnosed in the early stages, then the pathology can resolve itself. Relapses of alveolitis lead to the fact that the lung tissue undergoes irreversible changes. This worsens the prognosis, as well as the complications of alveolitis or its chronic course.









