Contents
Hepatocellular carcinoma
Hepatocellular carcinoma is the most common of the primary liver cancers. It affects a growing number of people in western countries, usually with cirrhosis or other liver disease. Despite the progress of treatments, it is too often fatal.
What is hepatocellular carcinoma?
Definition
Hepatocellular carcinoma (referred to by the abbreviation CHC) is cancer that develops from cells of the liver. It is therefore a primary cancer of the liver, as opposed to so-called “secondary” cancers corresponding to metastatic forms of cancer appearing elsewhere in the body.
Causes
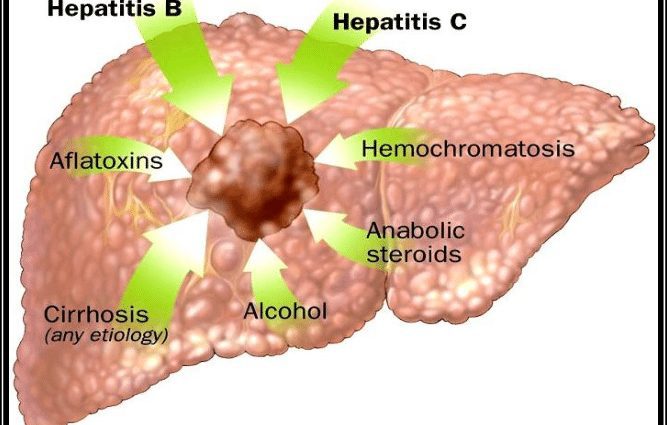
In the vast majority of cases, hepatocellular carcinoma is caused by hepatic cirrhosis, a consequence of chronic liver disease: viral hepatitis, alcoholic hepatitis, autoimmune hepatitis, etc.
This cirrhosis is characterized by chronic inflammation of the liver accompanied by destruction of liver cells. The uncontrolled regeneration of destroyed cells results in the appearance of abnormal nodules and fibrous tissue (fibrosis). These lesions promote tumor transformation of liver cells and carcinogenesis (formation of a malignant liver tumor).
Diagnostic
Screening for hepatic carcinoma is often based on the detection of a nodule on ultrasound in patients monitored for chronic liver disease.
In the event of an advanced tumor, the diagnosis may also be considered when symptoms appear.
POSTERS
The diagnosis is confirmed by further imaging tests. The doctor will order an abdominal scan (helical scan), sometimes an MRI and / or a contrast ultrasound.
The assessment of tumor extension can call for an abdominal MRI and a thoracic or thoraco-abdominal CT scan. Doppler ultrasound can be used to assess portal blood flow abnormalities as a consequence of cancer. More rarely, a PET scan will be performed to better characterize the tumor and look for possible dissemination outside the liver.
Biological examinations
In about half of hepatocellular carcinomas, blood tests show an abnormally high level of alfafoetoprotein (AFP), which is secreted by the tumor.
biopsy
Examination of tumor tissue samples helps to avoid diagnostic errors and to characterize the liver tumor to guide treatment.
The people concerned
Hepatocellular carcinoma is the most common primary liver cancer. It is the fifth leading cause of cancer in the world and the third leading cause of cancer death.
In Southeast Asia and Africa, it can affect quite young people with cirrhosis from hepatitis B.
In Western countries, where it is sometimes linked to hepatitis C but where it remains the consequence of alcoholic cirrhosis much more frequently, it increased sharply from the 1980s.
In France, the number of new cases discovered each year thus increased from 1800 in 1980 to 7100 in 2008 and to 8723 in 2012. This increase undoubtedly also partly reflects the improvement in diagnosis and better management of other complications of cirrhosis. According to the National Institute for Public Health Surveillance (InVS), the rate of appearance of new cases in 2012 was 12,1 / 100 in men and 000 / 2,4 in women.
Despite better control of the hepatitis B epidemic and the overall decline in alcohol consumption, hepatocellular carcinoma remains a major public health problem today.
Risk factors
An age over 55 years, male sex and advanced cirrhosis are the main risk factors for hepatocellular carcinoma. In France, excessive alcohol consumption remains the main risk factor for cirrhosis, and therefore liver cancer.
Obesity and its associated metabolic disorders, which promote fatty liver disease (“fatty liver”), are also linked to an increased risk of liver cancer.
Other risk factors may intervene:
- smoking,
- exposure to certain toxicants (aflatoxins, thorium dioxide, vinyl chloride, plutonium, etc.),
- infections with certain types of fluke,
- diabetes,
- hemochromatosis (genetic disorder inducing iron overload in the liver)…
Symptoms of hepatocellular carcinoma
Hepatocellular carcinoma can progress silently for a long time. Symptoms appear late, at an advanced stage of the tumor, and are often not specific to the cancer itself. They result from cirrhosis or obstruction of the portal vein and / or bile ducts.
Pain
It is most often a dull ache in the epigastric region. Sharp pains are rare.
Jaundice
Jaundice (jaundice), which causes the skin and whites of the eyes to appear yellowish, is caused by too much bilirubin (a bile pigment) in the blood.
Distension of the abdomen
Cirrhosis, as well as hepatocellular carcinoma itself, are causes of ascites, characterized by an effusion of fluid in the abdomen.
Other symptoms:
- abdominal hemorrhage by rupture of the tumor,
- disturbances of digestive functions (lack of appetite, gas, diarrhea or constipation, etc.),
- infections,
- shortness of breath caused by a large tumor pressing on the diaphragm
- general deterioration in health …
Treatments for hepatocellular carcinoma
The therapeutic management varies according to the characteristics of the tumor, in particular its extension, the state of the liver and the general state of health of the patient. In advanced cancers, the prognosis remains bleak despite advances in therapies.
Liver transplant
It offers a curative treatment for both the tumor and its cause – cirrhosis – and often allows healing, provided that the patient meets the criteria for graft allocation:
- localized tumor: 1 nodule measuring up to 6 cm in diameter, or 4 nodules less than 3 cm if the alphafoetoprotein level is less than 100 ng / ml,
- absence of vascular disease of the liver (portal or hepatic thrombosis),
- no contraindication: active alcoholism, patient who is too old or in poor health, associated pathologies, etc.
In France, around 10% of patients would be eligible for a transplant. In a context of shortage of grafts, it is carried out in 3 to 4% of them. Alternatives are sometimes possible, for example the transplant of a hemifoie resulting from a family donation or a deceased donor or that of a liver carrying an amyloid neuropathy, which functions correctly but can cause years of distance neurological disease.
The complications are those of any transplant.
Chemoembolization
This treatment can be a waiting treatment for a transplant, and can be repeated every two to three months. It combines chemotherapy injected through the arterial route with embolization, ie a temporary obstruction of the hepatic artery itself or of the branches which supply the tumor with “embolization agents”. In the absence of blood supply, tumor growth decreases, and the size of the tumor can even be reduced significantly.
Local destructive treatments
The methods of local destruction by radiofrequency (tumors of less than 2 cm) or microwaves (tumors of 2 to 4 cm) require good visibility of the tumor. These treatments are carried out in the operating room, under general anesthesia. There are contraindications, including ascites or too low a blood platelet count.
surgery
The choice of performing surgery to remove the tumor depends, among other things, on the location of the carcinoma and the general condition of the patient. Most often, the intervention is reserved for superficial tumors and not too large (the patient must keep enough healthy liver tissue). The efficiency is quite good.
External radiotherapy
External radiotherapy is an alternative to the local destruction of a hepatic carcinoma presenting a single nodule of less than 3 cm, especially in the upper part of the liver. It requires several sessions.
Drug treatments
Classical intravenous chemotherapy is not very effective, especially since the underlying liver disease requires low dosages. For the past ten years or so, targeted cancer therapies have been introduced in the treatment of hepatocellular carcinomas. Orally administered antiangiogenic agents (Sorafenib or other molecules) are used in particular, which prevent the development of micro-vessels feeding the tumor. These are essentially palliative treatments, which however make it possible to extend survival.
Prevent hepatocellular carcinoma
The prevention of hepatocellular carcinoma lies mainly in the fight against alcoholism. It is advisable to limit alcohol consumption to 3 drinks per day for men and 2 drinks for women.
Screening and management of hepatitis that causes cirrhosis also has a role to play. The prevention of sexual and intravenous contamination as well as the vaccination against hepatitis B are effective.
The fight against obesity contributes to prevention.
Finally, improving early diagnoses is an important issue in enabling curative treatments.