Contents
Gigantism
Gigantism is caused by excessive secretion of growth hormone during childhood, which results in very large height. This extremely rare condition is most often linked to the development of a benign tumor of the pituitary gland, the pituitary adenoma. In recent years, research has uncovered the frequent involvement of genetic factors. Treatment is difficult and often multimodal.
Gigantism, what is it?
Definition
Gigantism is a very rare form of acromegaly, a condition caused by excessive secretion of growth hormone, also called GH (for growth hormone), ou hormone somatotrope (STH).
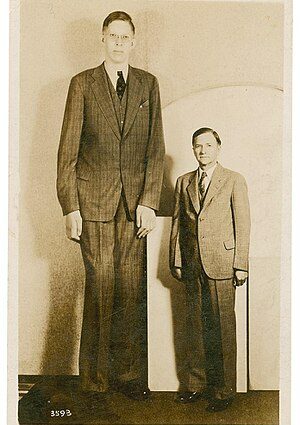
When it occurs before puberty (juvenile and infantile acromegaly), when the bone cartilages are not yet united, this hormonal abnormality is accompanied by excessive and rapid growth of the bones in length as well as of the whole body. and leads to gigantism.
Children with the condition are unusually tall, with boys reaching 2 meters or more in their late teens.
Causes
Normally, growth hormone is released into the blood by a small gland at the base of the brain called the pituitary gland. In children, its main role is to promote growth. The production of growth hormone by the pituitary gland is itself regulated by GHRH (growth hormone-releasing hormone), a hormone produced by the nearby hypothalamus.
Growth hormone hypersecretion in children with gigantism is most often due to the appearance of a benign tumor in the pituitary gland, called pituitary adenoma: the proliferation of hormone-producing cells explains its level abnormally high.
In less than 1% of cases, the pituitary gland is overactive because it is over-stimulated by GHRH, which is produced in excess by a tumor that can be located anywhere in the body.
Diagnostic
Gigantism is suspected in the face of markedly accelerated growth (the height growth curve is compared to the average curve), when the child is very tall compared to other members of his family. Clinical examination reveals other abnormalities associated with gigantism (see symptoms).
The diagnosis is confirmed by blood tests, which include repeated measurements of growth hormone as well as the glucose braking test – the rise in blood glucose levels following the absorption of a sugary drink induces normally a decrease in growth hormone secretion, not observed in subjects with gigantism.
Imaging exams are done to locate the tumor causing gigantism:
- MRI (magnetic resonance imaging) is the examination of choice to visualize a pituitary adenoma;
- the scanner is mainly used to look for tumors secreting GHRH in the pancreas, ovaries or adrenal glands;
- the radiography makes it possible to objectify the abnormalities of bone growth.
The presence of a pituitary adenoma can interfere with the functioning of the pituitary to varying degrees. In addition to growth hormone, it produces prolactin (lactation hormone) as well as other hormones whose role is to trigger secretions from the adrenal glands, the thyroid gland and the genital glands. A complete hormonal assessment is therefore necessary.
The tumor can also compress the optic nerves and induce visual disturbances, hence the need for a thorough ophthalmologic examination.
Other additional examinations may be requested to assess various dysfunctions that may be associated with gigantism.
The people concerned
Gigantism is much rarer than acromegaly affecting adults, although this condition itself is very infrequent (3 to 5 new cases per million inhabitants per year). In the United States, only a hundred cases of gigantism have been identified.
Gigantism predominates overall in boys, but some very early forms are predominantly female
Risk factors
Gigantism generally presents itself as an isolated and sporadic hormonal pathology, that is to say occurring outside any hereditary context. But there are rare cases of familial pituitary adenomas, gigantism can also be one of the components of hereditary multitumor syndromes, such as McCune-Albrigh syndrome, type 1 multiple endocrine neoplasia (NEM1) or neurofibromatosis. .
Several genetic and genomic abnormalities associated with pituitary gigantism, hereditary or not, have been identified in recent years. A large retrospective international study coordinated by the Belgian endocrinologist Albert Beckers, covering 208 cases of gigantism, thus highlighted the involvement of genetic factors in 46% of cases.
Symptoms of gigantism
In addition to their giant stature, children and adolescents with gigantism can present other manifestations related to their pathology:
- moderate (frequent) obesity,
- an exaggerated development of the volume of the skull (macrocephaly), associated or not with particular facial features (prognathism, frontal bumps, etc.)
- visual disturbances such as a change in the field of vision or double vision,
- abnormally large hands and feet, with thin fingers,
- peripheral neuropathies,
- cardiovascular disorders,
- benign tumors,
- hormonal disorders …
Treatments for gigantism
The management of children with gigantism aims to control their excessive secretion of growth hormone, which generally requires implementing several treatment modalities.
Surgical treatment
Surgical removal of the pituitary adenoma is preferred as a first-line treatment. This is a difficult operation, which can most often be performed nasally although it is necessary to open the cranium when the adenoma is large (macroadenoma).
When the tumor is too large or too close to important structures in the brain, it cannot be operated on.
Radiotherapy
X-ray irradiation may be recommended in addition to surgery to destroy any residual tumor cells and treat recalcitrant tumors (around thirty sessions). This technique is painless but can cause a hormonal imbalance responsible for various disorders.
Recently, the Gamma Knife radiosurgery technique has been introduced. Instead of the scalpel, it uses gamma radiation, much more powerful and much more precise than x-rays, to destroy the tumor in one sitting. It is reserved for small tumors.
Drug treatments
Molecules effective in reducing growth hormone secretion may be prescribed in conjunction with surgery and radiation therapy, especially if tumor removal is incomplete. The therapeutic arsenal includes analogues of somatostatin and dopamine, which are quite effective but can have significant side effects.