Contents
FSH or Folliculostimulating Hormone
The follicle stimulating hormone, or FSH, is a key hormone of fertility in both men and women. This is why during a fertility check-up, its rate is systematically checked.
What is FSH or Follicle Stimulating Hormone?
In women
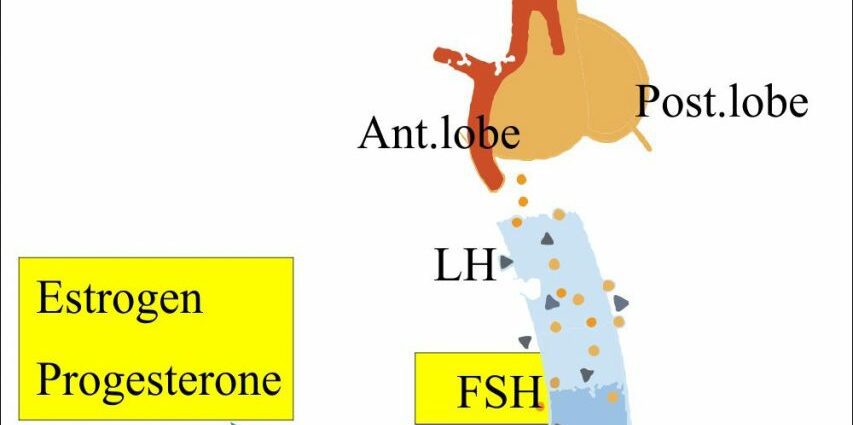
HSF occurs in the first phase of the ovarian cycle, known as the follicular phase. During this phase, which begins on the first day of menstruation and ends at the time of ovulation, the hypothalamus secretes a neurohormone, GnRH (gonadotropin releasing hormone). A chain reaction will follow:
- GnRH stimulates the pituitary gland, which in response secretes FSH;
- under the influence of FSH, around twenty ovarian follicles will start to grow;
- these maturing follicles will in turn secrete estrogen, responsible for thickening of the uterine lining in order to prepare the uterus to receive a possible fertilized egg;
- within the cohort, a single follicle, called the dominant follicle, achieves ovulation. The others will be eliminated;
- when the dominant preovulatory follicle is selected, estrogen secretion increases sharply. This increase causes a surge in LH (luteinizing hormone) which will trigger ovulation: the mature follicle ruptures and releases an oocyte.
At the center of this chain reaction, FSH is therefore a key hormone for fertility.
In humans
FSH is involved in spermatogenesis and the secretion of testosterone. It stimulates the Sertoli cells which produce sperm in the testes.
Why do an FSH test?
In women, a dosage of FSH can be prescribed in different situations:
- in the event of primary amenorrhea and / or late puberty: a coupled dosage of FSH and LH is carried out in order to distinguish between primary (ovarian origin) or secondary (high origin: hypothalamus or pituitary) hypogonadism;
- in case of secondary amenorrhea;
- in the event of a fertility problem, a hormonal assessment is performed with the dosage of different sex hormones: follicle stimulating hormone (FSH), estradiol, luteinizing hormone (LH), antimulleric hormone (AMH) and in some cases prolactin, TSH (thyroid), testosterone. Testing for FSH helps assess ovarian reserve and the quality of ovulation. It allows to know if the ovulation disorder or amenorrhea are due either to ovarian aging or to pituitary gland involvement.
- at menopause, the determination of FSH is no longer recommended to confirm the onset of pre-menopause and menopause (HAS, 2005) (1).
In humans
An FSH assay can be performed as part of a fertility assessment, in the face of a spermogram abnormality (azoospermia or severe oligospermia), in order to diagnose hypogonadism.
The FSH assay: how is the analysis carried out?
Hormonal measurements are taken from a blood test, not on an empty stomach.
- in women, the determinations of FSH, LH and estradiol are carried out on the 2nd, 3rd or 4th day of the cycle in a reference laboratory.
- in humans, the FSH dosage can be performed at any time.
FSH Too Low or Too High: Analysis of the Results
In women:
- a marked increase in FSH and LH indicates primary ovarian failure;
- a significant decrease in LH and FSH most often reflects damage to the pituitary gland, primary or secondary (tumor, pituitary necrosis, hypophysectomy, etc.);
- if FSH is high and / or estradiol low, a decrease in ovarian reserve is suspected (“early menopause”).
In humans:
- a high FSH level indicates testicular or seminiferous tubular damage;
- if it is low, “high” involvement (hypathalamus, pituitary) is suspected. An MRI and a complementary blood test will be performed to look for pituitary insufficiency.
Managing FSH Too High or Too Low to Get Pregnant
In women:
- in the event of ovarian failure or pituitary gland involvement, ovarian stimulation treatment will be offered. Its objective is the production of one or two mature oocytes. Different protocols exist, by oral route or injections;
- in the event of premature menopause, an oocyte donation may be offered.
In humans:
- in the event of hypogonatotropic hypogonadism (alteration of the hypotalamic-pituitary axis) with severe azoospermia or oligospermia, treatment to restore spermatogenesis will be prescribed. Two types of molecules can be used: gonadotropins with FSH activity and gonadotropins with LH activity. The protocols, which vary according to the patient, last 3 to 4 months, or even longer in certain situations.
- in the event of severe sperm alteration and certain azoospermia (for which it is possible to surgically remove the sperm from the epididymis or testis), IVF with ICSI may be offered. This AMP technique consists of injecting a sperm directly into the cytoplasm of the mature oocyte;
- sperm donation may be offered to the couple if spermatogenesis cannot be restored.