Contents
Fibrinolysis: definition, causes and treatments
Fibrinolysis occurs in physiological hemostasis, after blood coagulation, to eliminate the hemostatic clot formed by fibrin. Present in too large a quantity, it could lead to the formation of a clot in the circulation with the resulting risks. Definition, causes and treatments, let’s take stock.
What is fibrinolysis?
Fibrinolysis is a process of destruction which consists of the dissolution of intravascular clots under the action of plasmin. By this process, it rids the circulation of fibrin waste in the blood and therefore helps protect the body against the risk of thrombosis (blood clot).
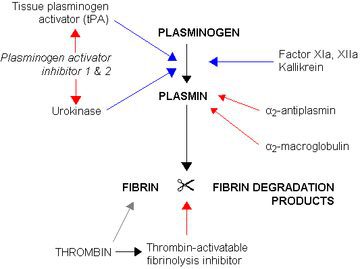
Plasmin, produced by the liver, is the main protein that activates fibrinolysis. Plasmin is converted to plasminogen by tissue plasminogen activator (tPA) and urokinase.
Plasminogen has a concordance for fibrin and is assembled in the clot during its formation (which will allow it to be broken down later). The change from plasminogen to plasmin takes place near the clot.
The fibrinolytic system must maneuver between breaking up the intravascular clots that form and not causing bleeding when the hemostatic clots and fibrinogen dissolve.
If the clot dissolves too quickly, by treatment, by disease or by an abnormality of hemostasis, it can then be responsible for sometimes significant bleeding.
Causes of fibrinolysis formation?
There are two types of fibrinolysis, primary and secondary fibrinolysis. Primary fibrinolysis occurs naturally, and secondary fibrinolysis occurs due to some external cause such as medication or a medical condition.
If the fibrin is present in too much quantity, it could cause the formation of a clot in the circulation, causing the risks of venous thrombosis (phlebitis) or arterial (ischemia).
Pathologies linked to fibrinolysis?
Defects in fibrinolysis lead to thrombophilia responsible for the excessive formation of life-threatening blood clots:
- Acute coronary syndrome (ACS) is coronary insufficiency caused by one or more blocked coronary arteries;
- Very recent myocardial infarction: intervention within the first three hours is preferable;
- Ischemic stroke in the acute phase;
- Pulmonary embolism with hemodynamic instability;
- Restoration of the patency of venous catheters (central venous catheters and dialysis catheters), in the event of an obstruction related to a developing or recently formed thrombus.
What treatments for fibrinolysis?
In all the cases mentioned above, the action of fibrinolytics will only be effective depending on the time of administration compared to the onset of the first symptoms.
The current standard treatment, fibrinolysis, must therefore be given as soon as possible and consists in injecting the patient with a tissue plasminogen activator which will attempt to dissolve this clot and thus lift the obstruction of the vessel.
Fibrinolytics precipitate the dissolution of intravascular clots and operate by modifying inactive plasminogen into active plasmin, an enzyme responsible for the deterioration of fibrin and which thus triggers lysis of the thrombus.
We distinguish:
- Streptokinase of natural origin is a protein produced by β-hemolytic streptococcus, therefore of exogenous origin and capable of causing the formation of antibodies;
- Urokinase is a protease, of natural origin, which acts directly on plasminogen;
- The derivatives of tissue plasminogen activator (t-PA), obtained by genetic recombination from the gene encoding t-PA, will directly transform plasminogen into plasmin by mimicking the action of t-PA. The t-PA derivatives are indicated by rt-PA (alteplase), r-PA (reteplase) and TNK-PA (tenecteplase).
Heparin and / or aspirin are frequently associated with treatment with fibrinolytics.
Diagnostic
Methods of exploring fibrinolysis.
Global tests: Dissolution time of euglobulins
The precipitation of euglobulins allows the sharing of fibrinogen, plasminogen and its protease inhibitor activators. The normal time is greater than 3 hours but in case of less time, we suspect “hyperfibrinolysis”.
Analytical tests
- Plasminogen assay: functional and immunological;
- TPA (tissue plasminogen) assay: immunoenzymatic techniques;
- Dosage of antiplasmin.
Indirect tests
- Determination of fibrinogen: this is an indirect assessment of fibrinolysis. With low fibrinogen, “hyperfibrinolysis” is suspected;
- Reptilase time and / or thrombin time: they are lengthened in the presence of fibrin degradation products;
- Determination of PDFs (Fibrin and fibrinogen degradation products): high in the event of activation of fibrinolysis;
- D-dimer assay: they correspond to PDF fragments and are high in the event of fibrinolysis.