Contents
Fetal abnormalities
The different types of fetal anomalies
The term fetal anomaly covers different realities. It could be :
- chromosomal abnormality: abnormality of number (with a supernumerary chromosome: trisomy 13, 18, 21), of structure (translocation, deletion), abnormality of sex chromosomes (Turner syndrome, Klinefelter syndrome). Chromosomal abnormalities affect 10 to 40% of conceptions, but due to natural selection (spontaneous miscarriages and mortality in utero) they affect only 1 in 500 newborns, about half of whom have Down’s syndrome (21);
- of a genetic disease transmitted by one of the parents. 1 in 1 newborns have it. The five most common diseases are cystic fibrosis, hemochromatosis, phenylketonuria, alpha-2 antitrypsin deficiency and thalassemia (XNUMX);
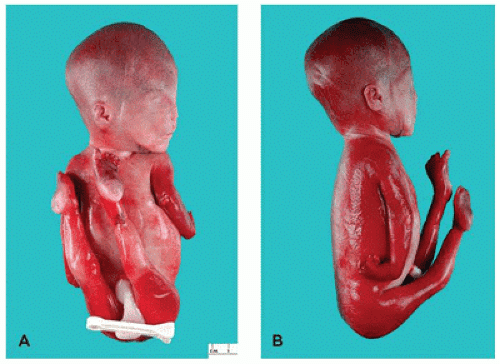
- a morphological malformation: cerebral, cardiac, genitourological, digestive, in the limbs, spine, face (cleft lip and palate). Exogenous causes (infectious, physical or toxic agents) explain 5 to 10% of cases, genetic or endogenous causes 20 to 30%. 50% of cases remain unexplained (3);
- an abnormality due to an infection contracted by the mother during pregnancy (toxoplasmosis, cytomegalovirus, rubella).
All of these pathologies represent 4% of live births, or 500 births in Europe (000).
Prenatal diagnosis to screen for fetal abnormalities
The pre-natal diagnosis is defined as the set of “medical practices intended to detect in utero in the embryo or the fetus, an affection of a particular gravity”. ”(Article L. 2131-1 of the public health code).
The three screening ultrasounds play a major first-line role in this prenatal diagnosis:
- the first, carried out between 11 and 13 weeks old, makes it possible to detect certain major malformations and participates in the screening of chromosomal anomalies by measuring nuchal translucency;
- the second so-called “morphological” ultrasound (22 SA) enables an in-depth morphological study to be carried out with the aim of highlighting certain physical morphological anomalies;
- the third ultrasound (between 32 and 34 WA) makes it possible to diagnose certain morphological abnormalities that appear late.
However, ultrasound cannot always detect fetal abnormalities. This ultrasound-based examination does not give an exact photograph of the fetus and its organs, but only images made of shadows.
Screening for trisomy 21 is systematically offered to expectant mothers, but not compulsory. It is based on the measurement of nuchal translucency (thickness of the neck) during ultrasound of the 12 AS and the determination in the maternal blood of serum markers (PAPP-A protein and b-HCG hormone). Combined with the mother’s age, these values make it possible to calculate a risk of Down’s syndrome. Beyond 21/1, the risk is considered to be high.
Examinations in case of suspicion of a fetal anomaly
A more in-depth prenatal diagnosis can be offered to the couple in different situations:
- screening examinations (ultrasounds, screening for trisomy 21) suggest an anomaly;
- the couple received genetic counseling (due to family or medical history) and a risk of fetal abnormality was identified:
- the mother-to-be has contracted an infection that is potentially dangerous for the fetus.
Prenatal diagnosis is based on the analysis of fetal cells to perform chromosome analysis, molecular genetic testing, or biological testing to identify fetal infection. Depending on the term of pregnancy, different tests will be used:
- trophoblast biopsy can be done from 10 WA. It consists of taking a sample of a very small fragment of the trophoblast (future placenta). It can be performed if a severe abnormality has been detected on ultrasound of the 12 WA or if there is a history of abnormalities during a previous pregnancy.
- amniocentesis can be performed from 15 weeks onwards. It involves taking amniotic fluid and makes it possible to diagnose chromosomal or genetic abnormalities, as well as to detect signs of an infection.
- Fetal blood puncture involves taking fetal blood from the umbilical vein of the fetus. It can be performed from 19 weeks old to establish a karyotype, for genetic research, an infectious assessment or a search for fetal anemia.â € ¨
A so-called “diagnostic” or “second-line” ultrasound is performed when a particular risk is identified by screening ultrasound, by history (genetic risk, diabetes, exposure to toxins, etc.) or biological screening. More anatomical elements are analyzed according to a specific protocol depending on the type of anomaly (5). This ultrasound is often performed by a specialist doctor working in a network with a multidisciplinary prenatal diagnosis center. An MRI can be performed as a second line, for example to explore the central nervous system or to determine the extent of a tumor or a malformation.
Management of fetal anomalies
As soon as a fetal anomaly is diagnosed, the couple is referred to a multidisciplinary prenatal diagnosis center (CPDPN). Approved by the Biomedicine Agency, these centers bring together different specialists in prenatal medicine: sonographer, biologist, geneticist, radiologist, neonatal surgeon, psychologist, etc. Management depends on the type of anomaly and its severity. It can be:
- surgery in utero or drug treatment of the fetus in utero, via the mother;
- a surgical intervention from birth: the mother-to-be will then give birth in a maternity hospital capable of performing this intervention. We speak of “transfer in utero”;
- when the fetal anomaly detected is considered by the CPDPN team as having a “high probability that the unborn child will have a condition of particular gravity deemed incurable at the time of diagnosis” (art. L. 2231-1 of the Public Health Code), a medical termination of pregnancy (IMG) is offered to parents, who remain free to accept it or not.
In addition, psychological care is systematically offered to the couple in order to overcome this difficult ordeal of the announcement of a fetal anomaly and, if necessary, an IMG.