Contents
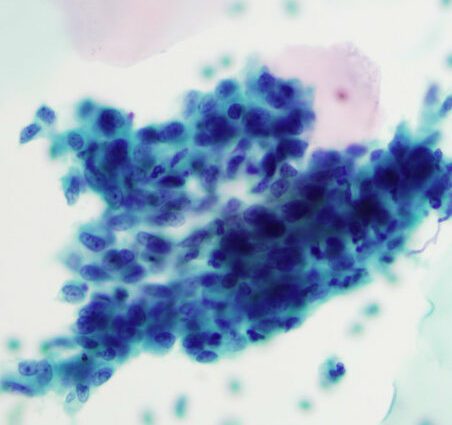
Endocervical cells
Endocervical cells, also called endocervical column cells, are one of the types of cells lining the cervix in women. Their presence on the smear indicates that the sample was taken in the right place and that its cytological analysis is therefore reliable.
Anatomy
Endocervical cells are cells that line the endocervical epithelium.
As a reminder, the cervix (lower part of the uterus that connects the body of the uterus to the vagina) is made up of two parts:
- endocervix refers to the inner part of the cervix that lines the duct leading to the uterus. It is covered by the glandular epithelium, made up of endocervical cells. Long and columnar in shape, they are also called endocervical columnar cells;
- the ectocervix, the external part of the cervix that connects it to the vagina, is covered by the squamous epithelium, made up of squamous cells.
The border area where the ecocervix and endocervix meet is called the junction zone (or squamocolumnar junction zone). It is also called the transformation zone, because it is there that precancerous lesions (dysplasias) cancerous lesions most often appear.
physiology
Endocervical cells are involved in the production of cervical mucus.
Anomalies / Pathologies
The junction area can be the site of various cellular modifications, or dysplasias. It is in fact the area most sensitive to human papillomavirus (HPV) viruses, and more particularly HPV 16 and 18, responsible for a large number of cancers of the cervix.
The most frequent lesions, called cervical intraepithelial neoplasia or CIN, however affect the squamous epithelium of the cervix and not the endocervical epithelium. Untreated, they can progress after several years to squamous cell carcinoma.
More rarely, the endocervical glandular epithelium and endocervical cells are affected. It will then be an adenocarcinoma in situ (AIS), the least common type of cervical cancer (15%). As the cells of the glandular epithelium shed little, its diagnosis is more difficult.
The two types of lesions (CIN and AIS) can be associated.
Treatments
Hysterectomy (surgical removal of the uterus) remains the standard treatment for adenocarcinoma in situ, but in young patients wishing to become pregnant, conservative treatment is sometimes possible. It is based on in-sano resection (with healthy margins) by conization of the lesions with a margin of more than 1cm, on a careful study of the operative part and close monitoring after treatment in order to detect any recurrence as quickly as possible.
Diagnostic
Pap smear
The cervico-vaginal smear is the standard examination of the cervix. It makes it possible to detect pre-invasive lesions or cancers at an early stage. As such, it is the key examination for cervical cancer screening. In its recommendations, the HAS (Haute Autorité de Santé) recommends performing cervico-uterine cytology in women aged 25 to 65 every 3 years after two normal cytologies performed one year apart.
The smear consists in taking vaginally, using a small brush, cells of the endocervix (endocervical cells) and cells of the ectocervix (squamous cells) in order to carry out a cytological analysis to find possible cellular abnormalities. To be reliable, the sample must contain sufficient of these two types of cells. This is a sign that it has been done on the junction area, an area at risk of pre-cancerous or cancerous lesions. As such, the presence of endocervical cells on the smear is a guarantee of reliability.
The smear results indicate either:
- the presence of endocervical columnar cells: this means that the junction area has been correctly removed. The smear is therefore reliable;
- the absence of endocervical columnar cells: the functional area was not sufficiently removed, the cytological analysis is therefore not sufficiently reliable. A new smear must be done.
Note that certain factors favor the absence of endocervical cells on the smear:
- menopause ;
- hormonal contraception;
- wearing an IUD (intrauterine device or IUD);
- an inflammatory condition;
- a history of conization or laser on the cervix;
- an anatomical peculiarity of the cervix.
The HPV test
In the event of an abnormal smear (ASC-US or ASC-H or AGC according to the Bethesda system), an HPV test is performed to check for the presence of the virus. It is done either on the initial smear if it was carried out in a liquid medium, or on a second sample if it was a smear on a slide.
Colposcopies
If the HPV test is positive, a colposcopy is performed. This examination, performed during a gynecological consultation, consists of observing the cervix with a colposcope (magnifying binocular magnifier) in search of abnormalities. The application of two dyes will react the abnormal lesions which will then appear colored. If there is a lesion, the gynecologist takes a biopsy of the suspicious area. The samples are then sent to the laboratory for anatomopathological analysis.
Conization
If the lesion is not accessible to biopsy, a conization will be performed. This surgical intervention, most often performed on an outpatient basis, consists of cutting and then removing the suspicious area in the form of a small cone. The part is then analyzed. Sometimes the adenoma in situ is diagnosed on a conization piece.