Contents
Diabetes insipidus
Diabetes insipidus is characterized by excessive urine production associated with intense thirst. It is possible to distinguish several types, the most common of which are neurogenic diabetes insipidus and nephrogenic diabetes insipidus. These do not have exactly the same characteristics but both reflect a regulatory problem in the kidneys. The body does not retain enough water to cover its needs.
What is diabetes insipidus?
Definition of diabetes insipidus
Diabetes insipidus is the consequence of a deficiency or insensitivity to the antidiuretic hormone: vasopressin. As part of the body’s normal functioning, this hormone is produced in the hypothalamus and then stored in the pituitary gland. After these two steps in the brain, vasopressin is released in the body to regulate the amounts of water in the body. It will act on the kidneys to reabsorb filtered water, and thus prevent its elimination in the urine. In this way, it helps to cover the body’s water needs.
In diabetes insipidus, vasopressin cannot play its role as an antidiuretic agent. Water is excreted in excess, which results in excessive urine production associated with intense thirst.
Types of diabetes insipidus
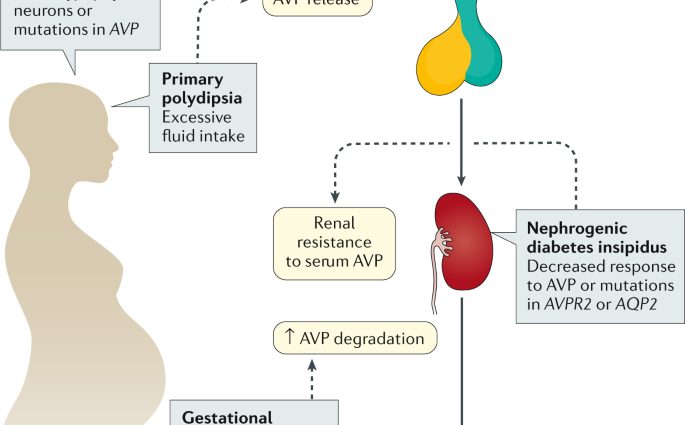
The mechanisms involved in diabetes insipidus are not always the same. This is why it is possible to distinguish several forms:
- neurogenic, or central diabetes insipidus, which is caused by insufficient release of antidiuretic hormone from the hypothalamus;
- nephrogenic, or peripheral, diabetes insipidus, which is caused by kidney insensitivity to antidiuretic hormone;
- gestational diabetes insipidus, a rare form occurring during pregnancy which is most often the consequence of a breakdown of vasopressin in the blood;
- dipsogenic diabetes insipidus which is characterized by a disorder of the thirst mechanism in the hypothalamus.
Causes of diabetes insipidus
At this stage, it should be noted that diabetes insipidus can be congenital (present from birth), acquired (following external parameters) or idiopathic (with an unknown cause).
Some of the causes identified to date include:
- head trauma or brain damage;
- brain surgery;
- vascular damage such as aneurysms (localized dilation of the wall of an artery) and thrombosis (formation of a blood clot);
- certain forms of cancer including brain tumors;
- autoimmune diseases;
- infections of the nervous system such as encephalitis and meningitis;
- tuberculosis ;
- sarcoidosis;
- polycystic kidney disease (presence of cysts in the kidneys);
- sickle cell anemia;
- sponge medullary kidney (congenital kidney disease);
- severe pyelonephritis;
- l’amylose ;
- the Sjögren syndrome;
- etc.
Diagnosis of diabetes insipidus
Diabetes insipidus is suspected upon excretion of large amounts of urine associated with extreme thirst. Confirmation of the diagnosis can then be based on:
- a water restriction test that measures urine output, blood electrolyte concentration and weight at regular intervals;
- urine tests to check the urine for sugar (characteristic of diabetes mellitus);
- blood tests to identify a high sodium concentration in particular.
Depending on the case, other additional examinations may then be considered to identify the cause of diabetes insipidus.
Many cases of diabetes insipidus are inherited. A family history of diabetes insipidus is a significant risk factor.
Symptoms of diabetes insipidus
- Polyuria: One of the typical symptoms of diabetes insipidus is polyuria. This is an excessive urine production exceeding 3 liters per day and can reach up to 30 liters in the most severe cases.
- Polydispsia: The second characteristic symptom is polydipsia. It is the perception of an intense thirst between 3 and 30 liters per day.
- Possible nocturia: It is common for polyuria and polydipsia to be accompanied by nocturia, a need to urinate at night.
- Dehydration: In the absence of appropriate management, diabetes insipidus can induce dehydration and functional impairment of the body. Hypotension and shock may be seen.
Treatments for diabetes insipidus
The management depends on many parameters including the type of diabetes insipidus. It may in particular include:
- adequate hydration;
- restricting the consumption of dietary salt and protein;
- administration of vasopressin or analogous forms such as desmopressin;
- the administration of molecules stimulating the production of vasopressin such as thiazide diuretics, chlorpropamide, carbamazepine, or even clofibrate;
- specific treatment targeting the identified cause.
Prevent diabetes insipidus
To date, no preventive solution has been established. In many cases, diabetes insipidus is inherited.