Contents
Cholestasis of pregnancy: symptoms and treatment of intrahepatic cholestasis
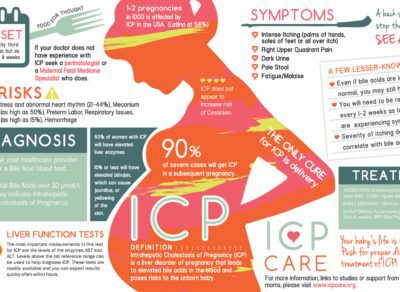
During pregnancy, itching in the stomach is frequent and not serious. But when they spread throughout the body, they can be a sign of a liver disorder. In its most severe forms, this cholestasis of pregnancy can be dangerous for the fetus. It must therefore be diagnosed and treated.
Definition of cholestasis of pregnancy
Intrahepatic cholestasis of pregnancy, better known as cholestasis of pregnancy, is the retention of bile in the liver. Instead of continuing their way through the digestive system, bile acids flow back into the blood where their concentration rises abnormally. This condition affects about 1% of pregnancies.
Causes and risk factors
Not all the mechanisms of cholestasis of pregnancy are known. But this hepatic pathology would occur when the hormonal modifications of pregnancy add to a genetically predisposed ground. The mother’s age and twinning have also been identified as risk factors.
Symptoms and diagnosis
Cholestasis of pregnancy causes intense itching (pruritus gestationnis), without apparent lesions such as eczema. They most often appear in the 3rd trimester, first in the palms of the hands and feet, before spreading to the whole body. 1 in 10 they are associated with jaundice (jaundice).
Any itching occurring during pregnancy therefore imperatively requires medical advice. To check for possible cholestasis of pregnancy, the doctor prescribes a blood test on an empty stomach in order to measure the transaminases and especially the serum bile acids. Cholestasis occurs if this liver test indicates a serum bile acid concentration greater than 10 µmoles / L. Above 14 µmoles / L, it is considered pathological and requires management.
What are the risks for mother and child?
Cholestasis of pregnancy usually has no impact on the mother’s health. The itching is accentuated at night, however, it can promote insomnia and fatigue.
On the other hand, the risks for the fetus are very real. Without knowing precisely why, the high concentrations of bile acids are indeed toxic for the latter. Beyond 40 µmoles / L, the fetal risk is considerably increased. The frequency of fetal deaths in utero at the end of pregnancy varies between 1 and 2% of cases. To limit their occurrence, premature deliveries are often necessary, with the associated risks.
The treatment
The treatment of cholestasis of pregnancy is based on taking ursodeoxycolic acid (AUDC) until delivery. Very well tolerated by the mother as well as by the fetus, this molecule makes it possible to limit the concentration of bile acids in the blood, thus reducing fetal risks and maternal itching. It is marketed under the names Délursan® and Ursolvan®.
Due to the fetal risk, hospitalization is generally necessary from the 36th week of amenorrhea in order to ensure optimal monitoring (liver tests, monitoring, ultrasound, etc.). The decision to induce childbirth after 37 weeks of amenorrhea is discussed on a case-by-case basis. At 39 weeks of amenorrhea, it is almost systematic.
The itching disappears spontaneously a few days after childbirth but the risk of recurrence is high. The following pregnancy should therefore benefit from close monitoring and may require immediate care in a level III maternity hospital.