Contents
Azoospermia: definition, causes, symptoms and treatments
During a fertility checkup of the couple, a spermogram is systematically carried out in the man. By evaluating different parameters of the sperm, this biological examination makes it possible to update various spermatic abnormalities, such as azoospermia, a total absence of sperm.
What is azoospermia?
Azoospermia is a sperm abnormality characterized by the complete absence of sperm in the ejaculate. It obviously leads to infertility in men, because in the absence of sperm there can be no fertilization.
Azoospermia affects less than 1% of men in the general population, or 5 to 15% of infertile men (1).
The causes
Depending on the cause, there are two types of azoospermia:
Secretory azoospermia (or NOA, for non-obstructive azoospermia)
Spermatogenesis is impaired or absent and the testes do not produce sperm. The cause of this spermatogenesis defect can be:
- hormonal, with hypogonadism (absence or abnormality in the secretion of sex hormones) which may be congenital (Kallmann-Morsier syndrome for example) or acquired, due in particular to pituitary tumors which alter the functioning of the hypothalamic-pituitary axis or after a treatment (eg chemotherapy);
- genetics: Klinefelter syndrome (presence of an extra X chromosome), which affects 1 in 1200 men (2), structural abnormality of the chromosomes, (microdeletion, i.e. loss of a fragment, of the Y chromosome in particular), translocation (one segment of the chromosome detaches and attaches to another). These chromosomal abnormalities are responsible for 5,8% of male infertility problems (3);
- bilateral cryptorchidism: the two testes have not descended into the bursa, which impairs the process of spermatogenesis;
- infection: prostatitis, orchitis.
Obstructive or excretory azoospermia (OA, obstructive azoospermia)
The testes do indeed produce spermatozoa but they cannot be exteriorized due to a blockage of the ducts (epididymis, vas deferens or ejaculatory ducts). The cause may be of origin:
- congenital: the seminal tracts have been altered from embryogenesis, resulting in an absence of the vas deferens. In men with cystic fibrosis, a mutation in the CFTR gene can cause the absence of vas deferens;
- infectious: the airways have been blocked following an infection (epididymitis, prostatovesiculitis, prostatic utricle).
Symptoms
The main symptom of azoospermia is infertility.
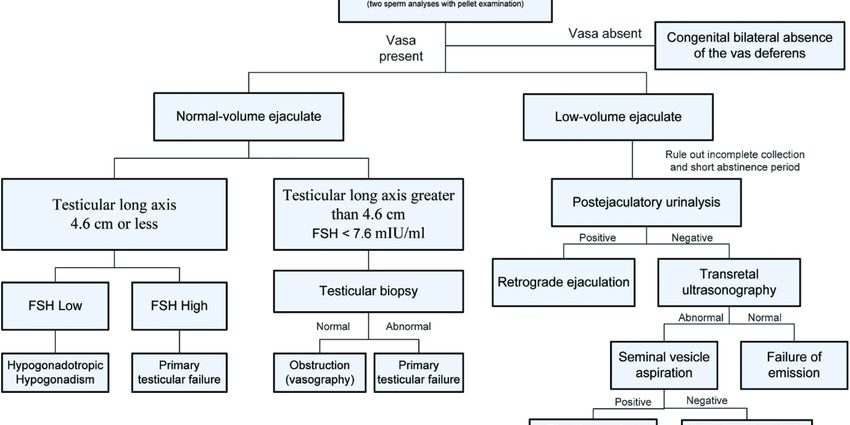
The diagnosis
The diagnosis of azoospermia is made during an infertility consultation, which in men systematically includes a spermogram. This examination consists of analyzing the content of the ejaculate (semen), evaluating various parameters and comparing the results with the standards established by the WHO.
In the event of azoospermia, no sperm is found after centrifugation of the entire ejaculate. To make the diagnosis, however, it is necessary to perform one, or even two other spermograms, each 3 months apart, because spermatogenesis (sperm production cycle) lasts about 72 days. In the absence of sperm production over 2 to 3 consecutive cycles, the diagnosis of azoospermia will be made.
Various additional examinations will be carried out to refine the diagnosis and try to identify the cause of this azoospermia:
- a clinical examination with palpation of the testes, measurement of testicular volume, palpation of the epididymis, of the vas deferens;
- seminal biochemistry (or biochemical study of sperm), in order to analyze various secretions (zinc, citrate, fructose, carnitine, acid phosphatases, etc.) contained in seminal plasma and originating from the different glands of the genital tract (seminal vesicle, prostate, epididymis ). If the pathways are obstructed, these secretions can be disturbed and biochemical analysis can help to locate the level of the obstacle;
- a hormonal assessment by blood test, comprising in particular an assay of FSH (follicle-stimulating hormone). A high FSH level indicates testicular damage; a low FSH level of high involvement (at the level of the hypothalamic-pituitary axis);
- serology by blood test, in order to look for an infection, such as chlamydiae, which may or may cause damage to the excretory tract;
- a scrotal ultrasound to check the testes and detect abnormalities of the vas deferens or the epididymis;
- a blood karyotype and genetic tests to look for a genetic abnormality;
- a testicular biopsy consisting of collecting, under anesthesia, a piece of tissue inside the testis;
- an X-ray or MRI of the pituitary gland is sometimes offered if an upper pathology is suspected.
Treatment and prevention
In the event of secretory azoospermia of hormonal origin following an alteration of the hypothalamic-pituitary axis (hypogonadotropic hypogonadism), hormonal treatment may be proposed to restore the hormonal secretions necessary for spermatogenesis.
In other cases, a surgical search for spermatozoa can be carried out either in the testes during the testicular biopsy (technique called TESE: TEsticular Sperm Extraction) if it is a secretory azoospermia, or in the testicular biopsy. epididymis (MESA technique, microsurgical epididymal sperm aspiration) if it is an obstructive azoospermia.
If sperm are collected, they can be used immediately after the biopsy (synchronous collection) or after freezing (asynchronous collection) during IVF (in vitro fertilization) with ICSI (intracytoplasmic sperm injection). This AMP technique involves directly injecting a single sperm into each mature oocyte. Since the sperm is selected and fertilization “forced”, ICSI generally provides better results than conventional IVF.
If no sperm can be collected, IVF with donated sperm may be offered to the couple.










Ibo ni ile iwosan yin wa