Contents
Asthenospermia: definition, causes, symptoms and treatments
Asthenospermia is a semen abnormality that affects the mobility of sperm. Less mobile, spermatozoa see their fertilizing power altered, with an impact on the fertility of men. The couple may then have difficulty conceiving.
What is asthenospermia?
Asthenospermia, or asthenozoospermia, is a sperm abnormality characterized by insufficient sperm mobility. It can alter the fertility of the man and reduce the chances of pregnancy for the couple because if they are not sufficiently mobile, the sperm cannot migrate from the vagina to the tube to fertilize the oocyte.
Asthenospermia can be isolated or associated with other semen abnormalities. In the case of OATS, or oligo-astheno-teratozoospermia, it is associated with oligospermia (sperm concentration below normal values) and teratozoospermia (too high a proportion of abnormally shaped spermatozoa). The impact on human fertility will be even greater.
The causes
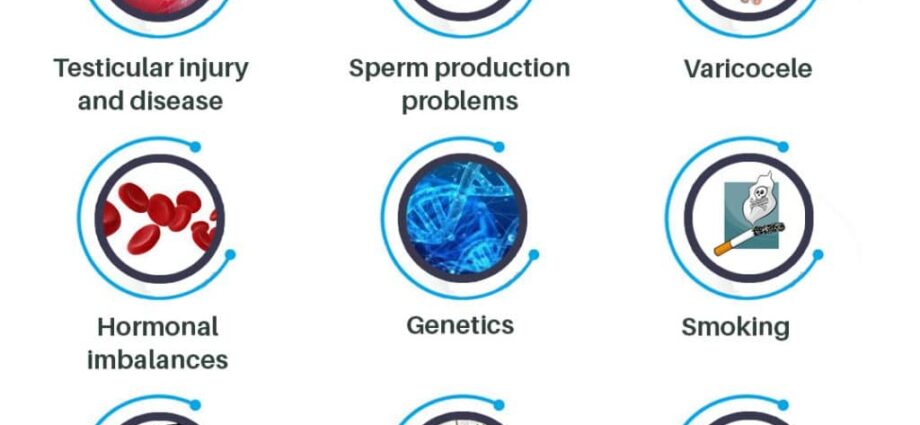
As with all semen abnormalities, the causes of oligospermia can be numerous:
- infection, fever;
- hormonal insufficiency;
- the presence of anti-sperm antibodies;
- exposure to toxicants (alcohol, tobacco, drugs, pollutants, etc.);
- a genetic abnormality;
- a varicocele;
- nutritional deficiency;
- general disease (kidney, liver);
- treatment (chemotherapy, radiotherapy, certain drugs)
Symptoms
Asthenospermia has no symptoms other than difficulty conceiving.
The diagnosis
Asthenospermia is diagnosed by the spermogram, a biological analysis of the sperm carried out systematically in men during the infertility assessment of the couple. During this examination, various parameters of the sperm are evaluated, including the mobility of the sperm. This is the percentage of sperm able to progress from the vagina to the tube to fertilize the oocyte. To evaluate this parameter, biologists check, on a drop of semen placed between two slides, the percentage of spermatozoa capable of rapidly crossing the field of the microscope in a straight line. They study this mobility at two points:
- within 30 minutes to one hour after ejaculation for so-called primary mobility;
- three hours after ejaculation for so-called secondary mobility.
Sperm mobility is then classified into 4 grades:
- a: normal, rapid and progressive mobility;
- b: reduced, slow or slightly progressive mobility;
- c: movements in place, not progressive;
- d: immobile sperm.
According to the threshold values defined by the WHO (1), a normal sperm must contain at least 32% of sperm with progressive mobility (a + b) or more than 40% with normal mobility (a). Below this threshold, we speak of asthenospermia.
To confirm the diagnosis, a second or even a third spermogram must be performed 3 months apart (the duration of a spermatogenesis cycle being 74 days) to confirm the diagnosis, because many parameters (infection, fever, fatigue, stress, exposure to toxins, etc.) can influence spermatogenesis and transiently alter the quality of sperm.
Other examinations complete the diagnosis:
- a spermocytogram, an examination consisting of studying the shape of the spermatozoa under a microscope in order to detect any morphological abnormalities. In the event of asthenospermia in this case, an abnormality at the level of the flagellum can impair the mobility of the sperm;
- a sperm culture to detect an infection of the semen that could affect spermatogenesis;
- a migration-survival test (TMS), consisting in selecting by centrifugation the best quality spermatozoa and evaluating the percentage of spermatozoa able to fertilize the oocyte.
Treatment and prevention for having a child
The management depends on the degree of asthenospermia, other possibly associated spermatic abnormalities, in particular at the level of sperm morphology, and the results of the various examinations, the origin of the asthenospermia (if it is found), the age of the patient.
In case of mild or moderate asthenospermia, treatment may be tried to improve the quality of the sperm. Antioxidant supplementation that could promote the increase in the number and mobility of spermatozoa, by reducing oxidative stress, which is an enemy of spermatozoa. An Iranian study (2) notably showed that supplementation with anti-oxidant coenzyme Q-10 improved the concentration and mobility of spermatozoa.
When it is not possible to treat the cause of asthenospermia or when the treatments do not give any results, different ART techniques may be offered to the couple depending on the situation:
- in vitro fertilization (IVF);
- in vitro fertilization with microinjection (IVF-ICSI).