Contents
Amenorrhea (or no periods)
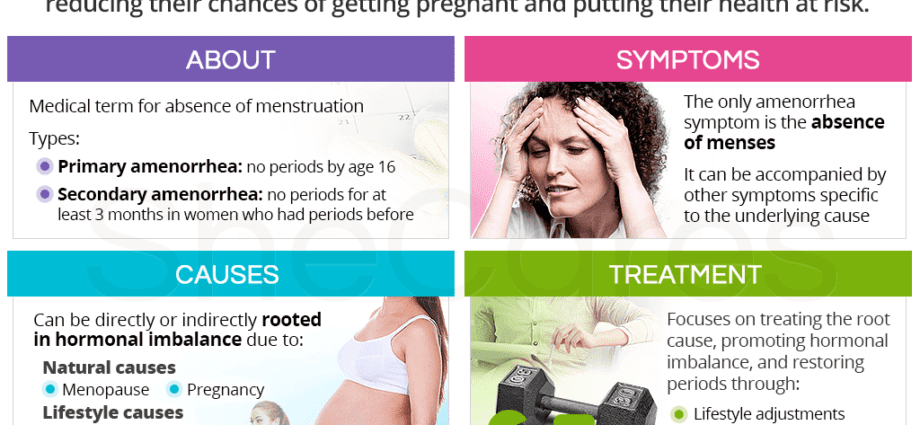
L’amenorrhea is theabsence of menstruation in a woman of childbearing age. The word “amenorrhea” comes from the Greek a for deprivation, melancholy for months and the rhea to sink.
From 2% to 5% of women would be affected by amenorrhea. This is a symptom which it is important to know the cause. The absence of periods is quite natural when, for example, the woman is pregnant, breastfeeding or approaching menopause. But outside of these situations, it can be a telltale sign of chronic stress or a health problem such as anorexia or a disorder of the thyroid gland.
Types of missed periods
- Primary amenorrhea: when at the age of 16, your period has not yet been triggered. Secondary sexual characteristics (development of the breast, hair in the pubis and armpits and distribution of fatty tissue in the hips, buttocks and thighs) may nevertheless be present.
- Secondary amenorrhea: when a woman has already had her period and stops having her period for one reason or another, for a period equivalent to at least 3 intervals of previous menstrual cycles or 6 months without menstruation.
When to consult when you don’t have a period?
Often times, not knowing why you have amenorrhea is worrying. The following people should see a doctor :
– women with primary or secondary amenorrhea;
– in the event of post-contraceptive amenorrhea, a medical evaluation is necessary if the amenorrhea persists for more than 6 months in women who have been on the contraceptive pill, who have worn a Mirena® hormonal IUD, or more than 12 months after the last injection of Dépo-Provera®.
Important. Sexually active women who are not taking hormonal contraceptives should have a pregnancy test if their period has been late for more than 8 days, even when they are “certain” that they are not pregnant. Note that bleeding that occurs with hormonal contraception (especially a false period generated by the birth control pill) is not proof of absence of pregnancy. |
Diagnosis of amenorrhea
In most cases, thephysical examination, for an pregnancy test and sometimes an ultrasound of the sexual organs is sufficient to guide the diagnosis.
An x-ray of the wrist (to assess pubertal development), hormone assays or chromosomal sex testing are done in rare cases of primary amenorrhea.
Causes of missing periods
There are many causes of amenorrhea. Here are the most frequent in descending order.
- The pregnancy. The most common cause of secondary amenorrhea, it must be the first suspected in a sexually active woman. Surprisingly, it often happens that this cause is ruled out without prior checking, which is not without risk. Some treatments indicated to treat amenorrhea are contraindicated in pregnancy. And with commercially available tests, diagnosis is simple.
- A minor delay in puberty. It is the most common cause of primary amenorrhea. The age of puberty is normally between 11 and 13 years old, but can vary a lot depending on ethnicity, geographic location, diet, and state of health.
In developed countries, delayed puberty is common in young women who are very thin or athletic. It seems that these young women do not have enough body fat to allow the production of estrogen hormones. Estrogens allow the lining of the uterus to thicken, and later menstruation if the egg has not been fertilized by a sperm. In a way, the bodies of these young women naturally protect themselves and signal that their physical form is inadequate to support a pregnancy.
If their secondary sexual characteristics are present (appearance of breasts, pubic hair and armpits), there is no need to worry before the age of 16 or 17 years. If signs of sexual maturation are still absent at the age of 14, a chromosomal problem (a single X sex chromosome instead of 2, a condition called Turner syndrome), a problem with development of the reproductive system or a hormonal problem.
- Breastfeeding. Often, breastfeeding women do not have a period. However, it should be noted that they can still have ovulation during this period, and therefore a new pregnancy. Breastfeeding suspends ovulation and protects against pregnancy (99%) only if:
– the baby takes the breast exclusively;
– the baby is less than 6 months old.
- The onset of menopause. Menopause is the natural cessation of menstrual cycles that occur in women between the ages of 45 and 55. The production of estrogen gradually decreases, causing periods to become irregular and then go away completely. You can ovulate sporadically for 2 years after you stop having your period.
- Taking hormonal contraception. The “periods” which occur between two packets of pills are not periods linked to an ovulatory cycle, but “withdrawal” bleeding when the tablets are stopped. Some of these pills reduce bleeding, which sometimes after a few months or years of taking it may no longer occur. Mirena® hormonal intrauterine device (IUD), injectable Depo-Provera®, continuous contraceptive pill, Norplant and Implanon implants can cause amenorrhea. It is not serious and demonstrates contraceptive efficacy: the user is often in a “hormonal state of pregnancy” and does not ovulate. It therefore has no cycle or rules.
- Stopping taking a contraceptive method (birth control pills, Depo-Provera®, Mirena® hormonal IUD) after several months or years of use. It may take a few months before the normal cycle of ovulation and menstruation is restored. It is called post-contraceptive amenorrhea. In fact, hormonal contraceptive methods reproduce the hormonal state of pregnancy, and can therefore suspend periods. These may therefore take some time to return after stopping the method, such as after pregnancy. This is particularly the case in women who had a very long (more than 35 days) and unpredictable cycle before taking the contraceptive method. Post-contraceptive amenorrhea is not problematic and does not compromise subsequent fertility. Women who find out they have fertility problems after contraception have had them before, but because of their contraception, they had not “tested” their fertility.
- The practice of a discipline or a demanding sport like marathon, bodybuilding, gymnastics or professional ballet. The “sportswoman’s amenorrhea” is thought to be attributable to the insufficiency of fatty tissue as well as to the stress to which the body is subjected. There is a lack of estrogen in these women. It can also be for the body not to waste energy unnecessarily since it often undergoes a low calorie diet. Amenorrhea is 4-20 times more common in athletes than in the general population1.
- Stress or psychological shock. So-called psychogenic amenorrhea results from psychological stress (death in the family, divorce, job loss) or any other type of significant stress (travel, major changes in lifestyle, etc.). These conditions can temporarily interfere with the functioning of the hypothalamus and cause menstruation to stop as long as the source of stress persists.
- Rapid weight loss or pathological eating behavior. Too low a body weight can lead to a drop in estrogen production and a cessation of menstruation. In the majority of women who suffer from anorexia or bulimia, periods stop.
- Excessive secretion of prolactin from the pituitary gland. Prolactin is a hormone that promotes mammary gland growth and lactation. Excess secretion of prolactin from the pituitary gland can be caused by a small tumor (which is always benign) or by certain medications (especially antidepressants). In the latter case, its treatment is simple: the rules reappear a few weeks after stopping the drug.
- Obesity or excess weight.
- Taking certain medications such as oral corticosteroids, antidepressants, antipsychotics, or chemotherapy. Drug addiction can also cause amenorrhea.
- Uterine scars. Following surgery to treat uterine fibroids, endometrial resection, or sometimes a cesarean section, there may be a significant decrease in menstruation, or even transient or long-lasting amenorrhea.
The following causes are much less common.
- A developmental anomaly sex organs of non-genetic origin. Androgen insensitivity syndrome is the presence, in an XY (genetically male) subject, of female-looking sex organs due to the absence of sensitivity of cells to male hormones. These “intersex” people with a feminine appearance consult at puberty for primary amenorrhea. The clinical and ultrasound examination allows the diagnosis: they do not have a uterus, and their sex glands (testes) are located in the abdomen.
- Chronic or endocrine diseases. An ovarian tumor, polycystic ovary syndrome, hyperthyroidism, hypothyroidism, etc. Chronic diseases that are accompanied by significant weight loss (tuberculosis, cancer, rheumatoid arthritis or other systemic inflammatory disease, etc.).
- Medical treatments. For example, surgical removal of the uterus or ovaries; cancer chemotherapy and radiotherapy.
- An anatomical anomaly sexual organs. If the hymen is not perforated (imperforation), this can be accompanied by painful amenorrhea in the pubescent girl: the first periods remain trapped in the vaginal cavity.
Course and possible complications
The duration of theamenorrheadepends on the underlying cause. In the majority of cases, amenorrhea is reversible and is easily treated (with the exception, of course, of amenorrhea related to genetic abnormalities, non-operable malformations, menopause or removal of the uterus and ovaries). However, when long-standing amenorrhea is left untreated, the cause may eventually reach the mechanisms of the patient. reproduction.
In addition, amenorrhea associated with a lack of estrogen (amenorrhea caused by demanding sports or an eating disorder) makes it more at risk of long-term osteoporosis – therefore of fractures, instability of the vertebrae and lordosis – since estrogen plays an essential role in preserving bone structure. It is now well known that female athletes who suffer from amenorrhea have lower bone density than normal, which is why they are more prone to fractures.1. While moderate exercise helps prevent osteoporosis, too much exercise has the opposite effect if it is not balanced by a higher calorie intake.