Brian Walsh
Almost every expert recommends it. And everyone accepts it. But what happens if we use it? What if our vitamin D supplements don’t help us at all?
Why do we lack vitamins?
Studies over the past few years have shown that a large percentage of the world’s population is low in vitamin D. However, the answer to the question of the reasons for this phenomenon looks strange.
Health care providers typically check patients’ vitamin D levels and note that they are low. Then they prescribe supplements. The patient comes back a few months later and the vitamin D level is still low. Then the doctor increases the supplements. In the past decade, vitamin D has become something of a miracle supplement, more studied than any other vitamin in the 21st century.
Hundreds of scientific studies show that vitamin D can help prevent diseases ranging from osteoporosis and autoimmune diseases to cardiovascular disease and cancer. It affects the recovery processes of the body, as well as our genes. Some have even suggested that vitamin D deficiency can lead to obesity. Meanwhile, statistics show that 40-50% of healthy adults and children lack vitamin D.
In fact, the last few years have seen a worldwide increase in rickets, and vitamin D deficiency is commonly found in malnourished children—even in industrialized countries!
The good news is that healthcare professionals are aware of this study and the risks associated with low vitamin D levels. Many doctors routinely prescribe high doses of vitamin supplements, 2000-10000 IU (International Units) per day, up to 50 IU per week, and sometimes more. .
Vitamin D obviously supports human health. But why aren’t we addressing the underlying reasons why our vitamin D levels regularly drop so low? And how safe is long-term high-dose vitamin D, really? What is vitamin D and how does it work?
The term “vitamin D” refers to a group of fat-soluble compounds that serve as prehormones, hormone precursors, and the active form of vitamin D is called calcitriol.
Among the best-known forms of vitamin D is vitamin D3 (cholecalciferol), found in fish, egg yolks, and cheese, and synthesized in the skin of humans and animals. Another common form, vitamin D2 (ergocalciferol), is synthesized by fungi and is most commonly used to fortify foods such as milk. We produce vitamin D in our skin when we go out in the sun – more specifically, when our skin is exposed to ultraviolet radiation. This initial form of vitamin D is called 7-dehydrocholesterol and is sent to the liver where it is converted to another, slightly more active form of vitamin D called 25-hydroxyvitamin D. This is the form of the vitamin that doctors test for when looking for a deficiency.
When vitamin D leaves the liver, it travels to the kidneys, where it is converted into a highly active form of vitamin D called calcitriol, or 1,25 dihydroxyvitamin D. This form is no longer considered a vitamin, but rather a steroid hormone. (You may be familiar with other steroid hormones such as estrogen, testosterone, and cortisol.)
The role of vitamin D in the body
As the name of the active form of vitamin D suggests, calcitriol helps in the absorption of calcium and other minerals in our body. Calcitriol increases the absorption of calcium from food in our digestive tract.
If we need more calcium, our kidneys can produce more of the active form of vitamin D, which raises our calcium levels by increasing the amount we absorb from our food.
Until recently, only a select few organs in our body were thought to have vitamin D receptors, called varistors. However, recent research shows that almost every cell in our body has vitamin D receptors, indicating a much more important role for this vitamin than we previously thought.
This new information helped us discover that vitamin D also affects our immune system and helps with cell differentiation, blood pressure regulation, insulin secretion, and more.
This brings us back to our original question: what does a vitamin D deficiency mean? It turns out that this is a signal – in a broader sense – that perhaps something has gone wrong in our bodily processes.
The Vitamin D Debate
25-hydroxyvitamin D, a form of vitamin D, is primarily produced by the liver and is generally accepted as the most reliable marker for assessing vitamin D levels. However, scientists cannot even agree on an optimal range for vitamin D levels.
Vitamin D deficiency is known to lead to bone abnormalities such as rickets and osteomalacia when blood levels are below 25 ng/mL. Some researchers believe a more optimal range is somewhere between 50 – 80 ng/mL. But there is no consensus on this issue.
In 2010, the National Institutes of Health (USA) set the recommended dietary intake for vitamin D at 600 IU daily for infants, children, and adults up to age 70. This is more than the previous recommendation of 200 IU per day. While this increase may seem significant, some people argue that it is not large enough to have “catastrophic” health consequences.
Sunny days… or not?
According to the National Institutes of Health, we can easily meet our body’s need for vitamin D simply by getting enough sunlight. If 30% of our skin is exposed (i.e. no clothes or sunscreen on) while in the sun for five to thirty minutes between 10 am and 3 pm three times a week, that’s enough.
But given the number of people who suffer from low vitamin D levels – even in sunny latitudes – you have to wonder if this recommendation is accurate. For those of us who live north of the 49th parallel, let’s just say that we won’t expose 30% of our unprotected skin to the sun very often in the winter.
If your levels are low, should you be taking supplements?
It is clear that vitamin D plays a number of important roles in the body and that vitamin D deficiency can harm you. Some studies show that the lower the vitamin D level, the higher the risk of all-cause mortality.
On the other hand, studies also show that the risk of total mortality actually rises as soon as vitamin D levels exceed 40 ng/mL. And, in general, we just don’t have unequivocal scientific evidence on the long-term safety of high doses of vitamin D. Perhaps before we start swallowing too many pills, we should evaluate whether we’re doing it. After all, medical science tends to be wrong often.
To get a better understanding of the issue, let’s look at some of the important relationships between vitamin D and other key nutrients.
Vitamin D and calcium
One of the potential risks of taking too much vitamin D is the development of hypercalcemia, or high levels of calcium in the blood. Vitamin D kills rats. Rodenticide is essentially a toxic dose of vitamin D—enough to kill an animal. However, hypercalcemia rarely appears without excessive doses of vitamin D, for the human body it would be somewhere in the range of 30,000-40,000 IU daily. Most people who take vitamin D supplements don’t take that much.
However, this does not necessarily mean that the dose taken is safe. Calcium levels in the body are so tightly regulated that abnormalities do not always show up in blood serum tests. But they can show up in other ways. One consequence can be hypercalciuria, otherwise known as calcium kidney stones.
Hypercalciuria occurs when the body tries to get rid of excess calcium and excretes it through the kidneys. Based on these findings, some researchers believe that high levels of supplemental vitamin D may lead to kidney stone formation.
Indeed, one study found that nursing home residents who took 5000 IU of vitamin D daily for six months showed an increased urinary calcium ratio, creatinine. It is speculated that excess calcium was excreted in the urine, probably because there was too much of it in their bodies.
On the other hand, another recent study found that among those whose vitamin D levels ranged from 20 to 100 ng/mL, there was no difference in the occurrence of kidney stones. Thus, the verdict is not clear. But kidney stones are not the only risk of too much calcium.
If the body cannot regulate calcium levels, the mineral can deposit in the body’s soft tissues, including the arteries. And, unfortunately, some research suggests that this is a real possibility when vitamin D levels get too high.
Three studies in particular have demonstrated increased arterial calcification in animals fed vitamin D supplements. And other studies show that high amounts of vitamin D can also damage the human cardiovascular system.
You know that high doses of vitamin D can increase the amount of calcium in the body’s soft tissues (such as the arteries), so you should take supplementation seriously.
Especially given the prevalence of cardiovascular disease in our society. So, now, you may be ready to toss your vitamin D in the trash can. But before we do that, again, we really need to consider why our vitamin D levels seem so inadequate that we tend to take supplements. Recall that vitamin D and calcium coexist in a delicate balance.
So maybe vitamin D levels are low due to too much calcium? And the body suppresses vitamin D production and conversion to minimize further increases in calcium. Why might our calcium levels be too high? Possibilities include magnesium deficiency, protein deficiency, liver dysfunction, and more. Let’s look at some of the possible interactions.
Vitamin D and Vitamin K
The name vitamin K comes from the German word koagulation. Coagulation refers to the process of forming a blood clot. This should hint to you that vitamin K plays an important role in the blood clotting process. Simply put, vitamin K allows the body to use calcium to carry out its clotting function. If vitamin K is not enough, the body cannot use calcium to form a clot.
In addition to participating in the clotting process, vitamin K also helps form and maintain our bones and teeth. It does this by activating a specific protein called osteocalcin, which helps the body use calcium.
In other words, the combination of calcium and vitamin K helps the body use calcium properly. And if we’re deficient in vitamin K, calcium can build up in our soft tissues.
People with low vitamin K levels suffer from atherosclerosis, the calcification of the arteries. And those who consume a lot of vitamin K (especially vitamin K2) are less prone to calcification of the arteries.
Indeed, a study in rats has shown that vitamin K2 (but not K1) supplementation not only inhibits arterial calcification, it can also remove 30-50% of the calcium that has already settled in the arteries. Unfortunately, this magical effect has not been tested on humans so far. I hope that now you can see the subtle dance that is happening inside of us. Vitamin D increases the level of calcium in the body. Vitamin K helps the body use calcium. So if we take large doses of vitamin D in the presence of a vitamin K deficiency, the long-term results can be disastrous.
Vitamin D and magnesium
Magnesium is an essential mineral involved in over 300 different processes in the body, including the ability to take in and use energy. Magnesium is also associated with vitamin D production and use. In particular, magnesium is able to modulate the sensitivity of our tissues to vitamin D.
But most importantly, it also helps maintain calcium balance. At least half of the population does not consume the recommended amount of magnesium. This may be due to the fact that magnesium content in the soil has dropped significantly over the past 50 years, making it increasingly difficult to meet our needs.
Because magnesium is used in vitamin D metabolism, some researchers believe that supplementing with large amounts of vitamin D may lead to even more magnesium deficiency. Interestingly, a relatively recent study showed a strong correlation between magnesium and vitamin D deficiency.
This study found that taking magnesium with vitamin D supplements was more effective in correcting vitamin D deficiency than taking vitamin D alone. Simply by increasing your intake of magnesium, you can reduce vitamin D deficiency-related deaths—without taking any vitamin D supplements. vitamin D
But, in addition to the interaction of vitamin D and magnesium, there are relationships of magnesium and calcium. And in a way, these two minerals have opposite effects. For example, calcium stimulates muscle contraction, while magnesium promotes muscle relaxation. Calcium increases platelet activity and blood clotting, while magnesium inhibits them.
Contrary to popular belief, individual levels of one of these minerals may be less important than the balance between them. An excess of calcium along with a deficiency of magnesium can cause problems such as an increase in calcium deposits in the arteries. Meanwhile, magnesium can prevent arterial calcification.
But what happens if you’re low on magnesium and decide to take vitamin D? There can be many negative effects, including—you guessed it—calcium deposits in the arteries.
Vitamin D and Vitamin A
In addition to gentle interactions with calcium and vitamin K, vitamin D also has a relationship with vitamin A in our bodies. The term “vitamin” refers to a group of fat-soluble compounds that promote growth and development, reproduction, immune system function, vision, skin health, and gene expression. Because fat-soluble vitamins can be stored in the body, they can reach toxic levels.
And here’s what’s interesting: it turns out that vitamin A can prevent the toxic effects of vitamin D, and vice versa. This means that if you are deficient in vitamin A, high doses of vitamin D can cause problems.
Meanwhile, some research suggests that increasing vitamin A may reduce the accumulation of calcium that tends to accompany high vitamin D levels. It may also protect against pathological calcification due to excess vitamin D.
By now, it’s clear that we should be careful with high doses of vitamin D. Up to 35% of the population is deficient in vitamin K. One study shows that vitamin D supplements may actually contribute to vitamin K deficiency, bone loss, and soft tissue calcification.
The researchers recommended taking vitamins A and K at the same time as vitamin D to improve the therapeutic effect of vitamin D and reduce its potential unwanted side effects.
The most worrisome of these is the effect of excess vitamin D on cardiovascular calcification. Cardiovascular disease has already become the number one killer in industrialized countries. We should not exacerbate this problem.
Take Vitamin D with Caution
We think we know a lot about the human body, but we don’t know much more. And when it comes to human physiology and biochemistry, and the role that nutrition and individual nutrients play in our bodies, we know even less.
Vitamin D deficiency is a real phenomenon and a real health risk, so we need to make sure we get enough of this important nutrient.
At the same time, we must also:
explore the possible long-term effects of high doses of vitamin D; consider the role of other key nutrients that interact with vitamin D;
always look for the root causes of any symptoms and deficiency.
What do we have to do?
1. Get enough vitamin D, but not too much.
Take about 1000 IU per day, but no more than 2000 IU per day during the winter months when you don’t get enough sunlight. It is safe, especially when other key nutrients are included, such as vitamin K, vitamin A, and magnesium. You can make sure you’re getting enough of them by taking a multivitamin.
Avoid overdose. While it is clear that the previous recommendation of 200 IU per day is probably too low, pending more solid research on the long-term benefits of high doses of vitamin D, beware of consuming too much.
Yes, it’s not a perfect system, especially during the winter months. But sunlight is still the best way for our bodies to get vitamin D.
2. Support Vitamin D
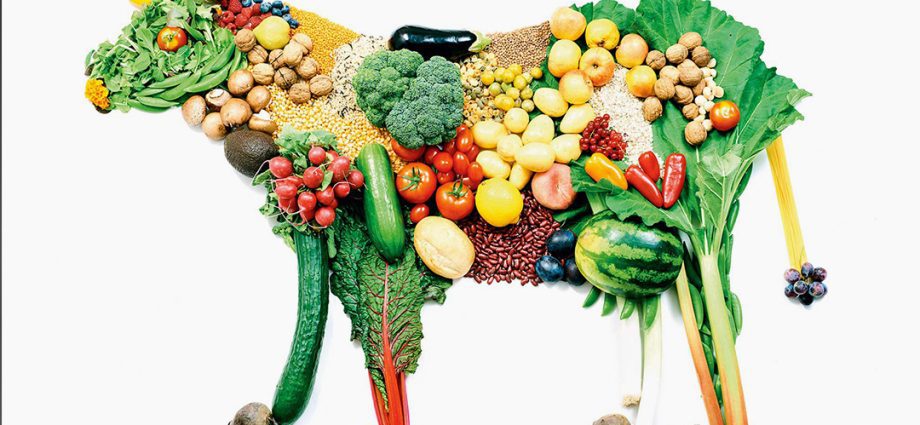
Be aware that other nutrients interact with vitamin D. Eat a variety of minimally processed foods to get magnesium, vitamin A, and vitamin K.
Eat greens and fermented foods. Kale, spinach, and chard are good sources of vitamin K1. They are also rich in magnesium. Sauerkraut and fermented cheeses are good sources of vitamin K2.
Eat colorful fruits and vegetables. A carotenoid, a form of vitamin A, is found in colorful fruits and vegetables. Butter, milk, and cheese are also good sources of the active form of vitamin A.
Maintain healthy intestinal flora. Vitamin K is converted in the gastrointestinal tract. Eat fermented foods, take probiotic supplements, avoid antibiotics unless absolutely necessary (a study found that broad-spectrum antibiotics can reduce vitamin K production by 75%).
Discuss all medications and supplements you take with your doctor or pharmacist. Many drugs, such as corticosteroids, prednisone, orlistat, statins, thiazide diuretics, can upset the delicate balance of vitamins and minerals in the body. Make sure you know all the side effects and interactions of the medications and “healthy” supplements you are taking.