Contents
Vasculitis of small capillaries
Vasculitis of small capillaries
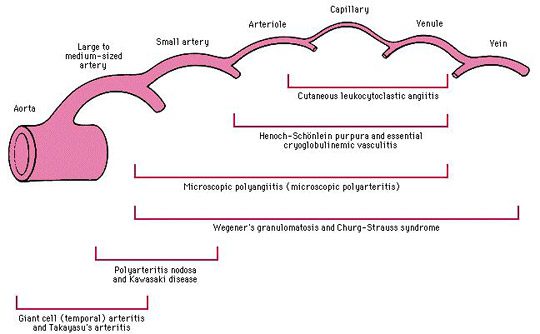
This is a large group of vasculitis of the wall of arterioles, venules or capillaries, the prognosis of which is very variable depending on whether it is pure or systemic cutaneous vasculitis.
The most common clinical aspect is the purpura (purplish spots that do not fade when pressed) bulging and infiltrated, especially in the lower limbs, aggravated by standing, which can take several forms (petechial and ecchymotic, necrotic , pustular…) or livedo, forming a sort of purplish mesh (livedo reticularis) or mottling (livedo racemosa) on the legs. We can also observe a Raynaud’s phenomenon (a few fingers turn white in the cold).
Purpura and livedo may be associated with other lesions on the skin (papules, nodules, necrotic lesions, bleeding bubbles), fixed urticaria that does not itch.
The presence of manifestations outside the skin constitutes a factor of gravity, showing the presence of vascular involvement in the organs:
- joint pain,
- abdominal pain, black stools, transit disorder,
- peripheral neuropathy
- edema of the lower limbs,
- Hyper Blood Pressure,
- breathing difficulties, asthma, coughing up blood …
The doctor prescribes examinations aimed at looking for a cause and signs of seriousness: blood test with blood cell count, search for inflammation, liver and kidney tests, etc., search for blood in the stool and x-rays according to the call points (lung x-ray in the event of breathing difficulties, etc.).
Vasculitis triggered by infection:
- bacterial: streptococcus, gram-negative cocci (gonococcus and meningococcus)
- viral: hepatitis, infectious mononucleosis, HIV, etc.
- parasitic: malaria …
- fungal: Candida albicans …
Vasculitis associated with immunological abnormalities
- Type II (mixed monoclonal) and III (mixed polyclonal) cryoglobulinemia, associated with autoimmune disease, infection (especially hepatitis C) or blood disease
- Hypocomplementémie (Mac Duffie’s urticarienne vascularite)
- Hyperglobulinémie (Waldenström’s hyperglobulinémique purple)
- Connectivitis: lupus, Gougerot-Sjögren syndrome, rheumatoid arthritis …
- Vasculitis of blood diseases and malignancies
- Leukemia, lymphoma, myeloma, cancer
- Vasculitis associated with ANCA (anti-neutrophil cytoplasmic antibodies)
Micro Poly Angéite or MPA
Micropolyangiitis (MPA) is a systemic necrotizing angeitis whose clinical signs are very similar to those of PAN.
MPA is associated with ANCA of the anti-myeloperoxidase (anti-MPO) type and it typically gives rise to rapidly progressive glomerulonephritis and pulmonary involvement which is absent in PAN.
The treatment of MPA as for PAN begins with corticosteroid therapy, sometimes combined with immunosuppressants (cyclophosphamide in particular)
Wegener’s disease
Wegener’s granulomatosis is a vasculitis the onset of which is generally marked by ENT or respiratory symptoms (sinusitis, pneumopathy, etc.) resistant to antibiotic treatments.
Classically, diffuse ENT (destructive pansinusitis), pulmonary (parenchymal nodules) and renal (crescent pauci-immune necrotizing glomerulonephritis) involvement produces the classic triad of Wegener’s granulomatosis.
The cutaneous-mucous membrane affects approximately 50% of patients: purpura (purplish spots which do not disappear when pressed) bulging and infiltrated, papules, subcutaneous nodules, skin ulcerations, pustules, vesicles, hyperplastic gingivitis …
ANCA is a diagnostic and evolutionary test for Wegener’s granulomatosis, with diffuse cytoplasmic fluorescence (c-ANCA), finely granular with perinuclear enhancement and / or purely perinuclear fluorescence (p-ANCA).
The management of Wegener’s granulomatosis, which can sometimes be considered a medical emergency, should be carried out in a specialized hospital setting, by a combination of cortisone and oral cyclophosphamide.
Churg and Strauss disease
Asthma is a major and early criterion of this vasculitis, which it precedes on average by 8 years before the first signs of vasculitis (neuropathy, sinus disorders, etc.) and which persists afterwards.
Blood tests show in particular a clear increase in eosinophilic polynuclear white blood cells
Treatment of Churg and Strauss disease begins with corticosteroid therapy, sometimes combined with immunosuppressants (especially cyclophosphamide)
Our doctor’s opinion
Infiltrated purpura (purplish, somewhat thick patches that do not fade with finger pressure) is the key sign of vasculitis. Unfortunately, this sign is not always present and the variability of unspecific clinical signs often makes diagnosis difficult for doctors. Likewise, it is often difficult to find a cause to treat in small vessel vasculitis, which is by far the most important case encountered in current practice compared to medium and large vessel vasculitis: about half of small vessel vasculitis. vessels have no cause found during the biological and radiological explorations that the doctor performs to seek an etiology. We often speak of “allergic vasculitis” or “hypersensitivity vasculitis” or rather “cutaneous vasculitis of small vessels of idiopathic caliber”. Dr. Ludovic Rousseau, dermatologist |
Landmarks
French Vasculitis Study Group: www.vascularites.org
Dermatonet.com, information site on skin, hair and beauty by a dermatologist
MedicineNet : http://www.medicinenet.com/vasculitis/article.htm