Contents
Transfusion-transfused syndrome: a complication of monochorionic pregnancies
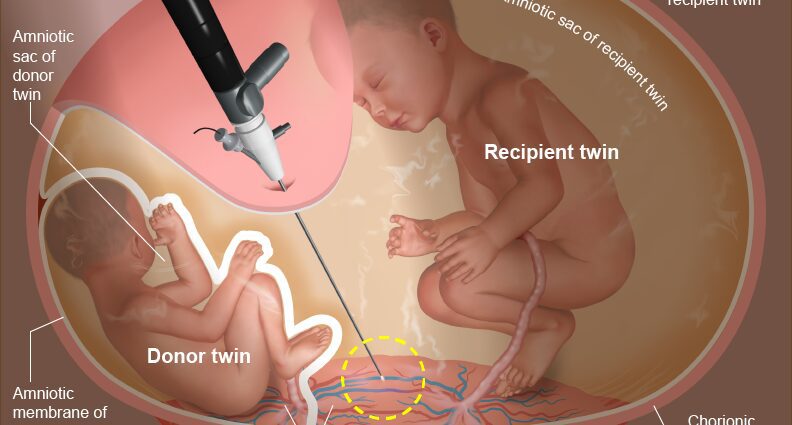
It is said that a twin pregnancy is monochorial when both twins share the same placenta (or chorion). It can be biamniotic, if the twins each develop in an amniotic sac, or monoamniotic if there is only one amniotic pouch for both fetuses.
La monochorial twin pregnancy implies that two umbilical cords are connected to the same placenta. These cords are linked together by blood vessels. But in 15 to 30% of cases, these connections (called anastomoses) will cause an imbalance in blood exchange. One of the twins will become the transfuser while the other will be the transfused. The blood of the donor twin passes into the blood of the recipient twin. To fight against this imbalance, regulatory mechanisms will be put in place and give rise to what is called the transfusion-transfused syndrome (STT).
Symptoms of a transfusion-transfused syndrome
Le twin transfused, who has an overload of blood volume, will try to compensate for it by increasing his urine production, which creates an excess of amniotic fluid (hydramnios). This transfused twin will usually be larger than his co-twin.
Le twin transfusionistconversely, has a decrease in blood pressure, a small bladder and sometimes anemia, due to the lack of blood. This donor twin produces little urine and therefore little amniotic fluid (oligoamnios). It is this twin who is particularly vulnerable and presents a high risk of in utero mortality.
In addition, this configuration increases the risk of miscarriage, because the uterus may believe that it has come to term given the large amount of amniotic fluid.
Diagnosis of transfusion-transfusion syndrome
The diagnosis of TTS is usually made by an ultrasound during the second trimester of pregnancy. Since he notes that the pregnancy is monochorial, the obstetrician-gynecologist will set about verifying certain data, including the amount of amniotic fluid and the size of each twin’s bladder.
When the practitioner observes a difference in amniotic fluid between the two fetuses (or a very large amount of overall amniotic fluid if the pregnancy is monochorial monoamniotic), with one fetus evolving in a lot of amniotic fluid and the other not, as well as a large bladder in the first and almost non-existent in the second, it will be able to validate the presence of a transfusion-transfused syndrome. When the twin transfusionist evolves in a particularly weak amniotic fluid, it is pressed against the uterine wall. Weight difference between twins strengthens diagnosis, although this discrepancy is not systematically present. Finally, in women, a distended uterus and excessive weight gain, linked to excess amniotic fluid, should suggest a transfusion-transfused syndrome.
Transfusion-transfused syndrome: the treatment
Nowadays, the one and only treatment for a transfusion-transfused syndrome is surgery. It was developed in France by Prof. Yves Ville, obstetrician gynecologist and Coordinator of the Reference Center for fetal-fetal transfusion syndrome at Necker Hospital (Paris), around twenty years ago and is carried out in 11 reference centers in France. Surgery involves inserting a small telescope into the uterus under local or epidural anesthesia, in order to access the amniotic sac of the transfused twin. The gynecological surgeon will then locate the vessels common to the two fetuses and coagulate them using a laser fiber. The excess amniotic fluid will also be drained, and an extract can be analyzed if you have given your consent, for a karyotype (analysis of chromosomes and detection of abnormalities). The operation will restore a balance of exchanges between the twins, and of “ pretend that these twins are bichorial, each with a part of the placenta for themselves », Specifies Professor Yves Ville. This treatment makes it possible 8 times out of 10 to have at least one of the two babies alive and without sequelae. In 35 to 50% of cases, the two babies survive, but we still deplore 20% of the deaths of the two twins, half of them by premature delivery linked to the trauma of the medical act.
Following the operation, the doctor will perform a control ultrasound to ensure fetal vitality, that there is no blood in the amniotic fluid, and to measure the amount of amniotic fluid remaining. The incision on the stomach is sutured with one point and medication is prescribed for abdominal pain. The patient is usually kept in the hospital under surveillance for 24 to 48 hours.
Finally, the National College of Obstetrician Gynecologists recommends, in the absence of complications after the operation, to schedule delivery from 34 weeks of amenorrhea (WA) and no later than 37 WA.