Contents
Treatment of asthma
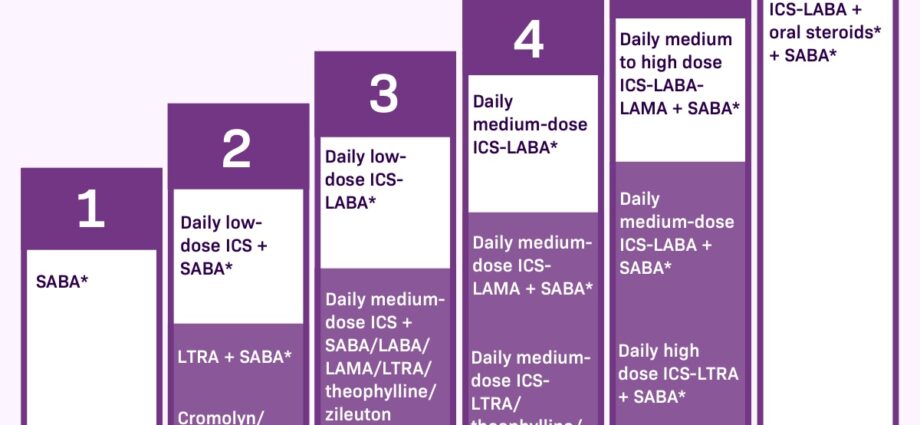
THEasthma is often a chronic disease which requires regular treatment, even between attacks. The pharmaceuticals to control asthma do not provide a definitive cure. They make breathing easier by increasing the opening of the bronchi (bronchodilation) and reducing inflammation. Most of them get caught by inhalation, which allows them to act quickly, with the fewest possible side effects. The doctor also tries to give the smallest dose of medication for symptom control with the best tolerability of the treatment.
Yet despite the effectiveness of treatments, 6 in 10 people with asthma fail to control their symptoms. The main causes are poor understanding of the disease, fear of Side effects and forgetting medications. However, the side effects of treatments taken by inhalation are minimal compared to the risks associated with severe and frequent asthma attacks.
Asthma treatment: understand everything in 2 min
Inhalation technique. The use of inhalers seems simple, but it requires a certain technique to be effective. However, less than half of asthmatics use their inhaler correctly67. The different inhalers (metered dose inhalers, dry powder inhalers and nebulizers) each have a specific mode of use. The doctor and pharmacist can explain the right actions to you. |
- Metered aerosols. You must shake the aerosol well and hold it vertically. After slowly emptying the lungs, breathe in slowly and very deeply through your mouth, triggering the aerosol during the first second of inspiration. You should then hold your breath for 5 to 10 seconds, then breathe out slowly.
- Dry powder inhalers (eg: Turbuhaler®). These systems are simpler to use because they do not require coordinating inspiration and triggering. You have to inhale as hard and quickly as possible, block your breathing for 10 seconds and exhale outside the inhaler.
- Inhalation chambers. They are used with a metered dose inhaler in children under 8 years of age and the elderly. In young children, inhalation is done with a face mask, which should be kept on the face for at least 6 calm breaths.
People with asthma are increasingly called upon to monitor their respiratory condition. For example, people with severe asthma, can measure their peak expiratory flow at home (peak flow) in order to adjust their treatment themselves according to the results. Training must have been taken beforehand.
pharmaceuticals
There are 2 categories of pharmaceuticals to control asthma symptoms. The first, called crisis or rescue medications, should be taken in case of symptoms. They have an immediate relief action, but do not calm the inflammation of the bronchi.
Other drugs are the control or background treatment. They should be taken every day, even in the absence of respiratory discomfort as soon as the asthma is moderate and persistent. They make it possible to reduce the inflammation of the bronchi and to space out the attacks. If not taken regularly, the frequency and severity of attacks increases, as does the need for rescue medication.
Many people with asthma do not fully understand the difference between crisis treatment and control treatment. Make sure you understand what each of your medications is for and how often you should use them. |
Crisis (or rescue) treatment
Crisis medications are referred to by different terms, including bronchodilators fast-acting or beta2 agonists short-acting. They are used only to relieve the symptoms of an attack (cough, chest tightness, wheezing and shortness of breath) or before exercise in asthma on exertion. In mild, intermittent asthma, seizure therapy may be the only medication needed.
These drugs include salbutamol ((Ventoline®, Ventilastin®, Airomir®, Apo-Salvent®, Novo Salmol®) or the terbutaline (Bricanyl®). They are taken by inhalation and widen the airways very quickly, 1 to 3 minutes. There are few side effects if used occasionally, but in high doses they can cause tremors, nervousness and rapid heartbeat. When you feel the need to take it often (usually more than 3 times a week), it means that asthma is not sufficiently controlled. It is then necessary to resort to background drugs to treat the inflammation.
For someone with asthma, it is important to always carry their bronchodilator with them, as an asthma attack can happen anywhere. It should be taken at the first symptoms of an attack and wait at least 30 seconds between 2 inhalations. |
Ipratropium bromide inhalation (rarely). It is an anticholinergic that blocks the action of a chemical that causes muscle in the airways to contract. Less effective than inhaled beta2 agonists, it is sometimes used in cases of intolerance to them. It takes 1 to 2 hours for maximum effect.
Drugs as a basic (control) treatment
Unlike seizure medications or rescue medications, DMARDs (control) medications do not immediately relieve symptoms. They work slowly and are effective in the long term in reducing inflammation and the frequency of seizures. That is why it is important to take them daily.
Corticosteroids. Corticosteroids decrease inflammation of the airways and therefore the production of mucus. They are usually taken in small doses as an inhalation (spray), on a daily basis (for example, Alvesco® and Pulmicort®). The doctor prescribes the lowest effective dose possible. They can also be taken as tablets in severe asthma for a short period of a few days (example: prednisolone, methylpredinosolone). Whether taken by inhalation or in tablets, they work the same way, but inhalation allows for much lower doses, a much more localized action and therefore fewer side effects. This class of drugs is the most effective in controlling asthma. Their effect is felt after a few days of use.
Adverse reactions
Taken by inhalation and in moderate doses, corticosteroids have few side effects, even if taken for a long time. Hoarseness and hoarseness or the appearance of muguet (or candidiasis, caused by yeast forming white patches on the tongue) are the most common side effects. Therefore, you should rinse your mouth after inhaling each dose. Corticosteroid tablets have stronger long-term side effects (weakening of the bones, increased risk of cataracts, etc.). They are reserved for cases of severe asthma, associated with other treatments.
Long-acting bronchodilators. These are prescribed in combination when inhaled corticosteroids alone are not sufficient to control asthma symptoms. The beta2 agonists long-acting causes bronchodilation for 12 hours. Their effectiveness can be rapid in 3 to 5 minutes as the formoterol® (ex Foradil®, Asmelor®) or slower after 15 minutes like the salmeterol (Serevent®). They are used in combination with a corticosteroid. There are inhalers that combine the two types of drugs like Seretide® (fluticasome / salmeterol). Combinations with formoterol (Symbicort®, Innovair® and Flutiform®) can also be used as a rescue medication, although they also act on inflammation in the long term.
The Antileukotrienes. Taken orally, they reduce inflammation caused by leukotrienes, substances contributing to the inflammatory response.In France, an antileukotrienes is available: montelukast (Singulair®). In Canada, there is also lezafirlukast (Accolate®). They can be used alone or in combination with inhaled corticosteroids. They are indicated to prevent asthma on exercise, in mild asthma, for people whose asthma is not controlled by inhaled corticosteroids alone, and for those who misuse their spray.
Theophylline. It is the oldest of the bronchodilators (eg: Theostat®). It is rarely used today, because effective dosage without side effects is difficult to find. It can be prescribed as a tablet to take with the evening meal in people who have difficulty taking the sprays.
Anti-immunoglobulin E. This class of drugs is intended to treat severe allergic asthma in people whose asthma is difficult to control with other treatments. Omalizumab (Xolair®) is the only drug in this class available in 2015. It is administered as subcutaneous injections once or twice a month.
He is really important to use a controller medication as directed by your doctor, even if there are no symptoms. Without regular use, inflammation of the bronchi persists and asthma attacks may be more frequent. |
The opinion of the doctor, Dr Annabel Kerjan pulmonologist:
When a person has asthma, they should not accept having symptoms without doing anything. You should not, for example, tolerate shortness of breath, a small cough, difficulty breathing at night. The disease should not be allowed to evolve, because if we tire of it without treating it, because it can degrade the bronchi over time, leading to a permanent worsening of the symptoms, and in severe cases frequent secondary infections and hospitalizations. It is better to find with your doctor the minimum effective treatment.
This is especially important for parents of children with asthma. They are often reluctant to give medicine to their children and this is understandable. But in this case, they are wrong. These children must be given the chance to properly develop their respiratory capital in order to have it available in adulthood. And then, a child who has signs of untreated asthma sleeps poorly, has difficulty in sports and grows less well. Whereas with treatment, he feels better and preserves his bronchi for the future.