Contents
Tracheotomy
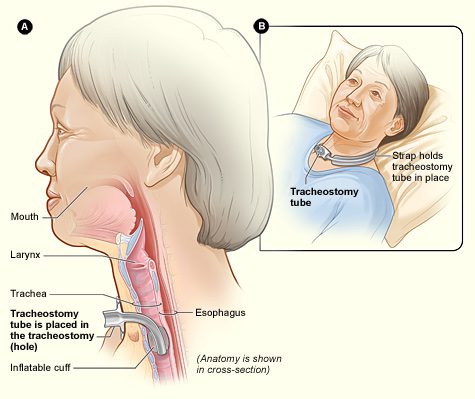
A tracheostomy is a surgical opening of the trachea to improve ventilation using a ventilator. This intervention can be carried out in a certain number of situations and in particular in intensive care.
What is a tracheostomy?
A tracheostomy consists of creating a small opening in the larynx and inserting a small cannula into it, which improves ventilation (entry and exit of air into the lungs), with or without a machine. This gesture bypasses the upper respiratory tract (nose and mouth). Air no longer needs to pass through the nose or mouth to reach the lungs. The tracheostomy can be permanent or temporary.
How is a tracheostomy performed?
Preparing for a tracheostomy
When the tracheostomy is not performed in an emergency context, it is preceded by an anesthesia consultation.
How is a tracheostomy performed?
A tracheostomy can be performed surgically under general anesthesia or percutaneously under local anesthesia.
For a surgical tracheostomy, an incision is made at the level of the trachea between the 2nd and 4th cartilage rings. A tracheostomy cannula is then inserted into the trachea through this orifice.
A percutaneous tracheostomy is done under local anesthesia, sometimes with additional sedation, at the bedside of the patient in intensive care and not in the surgical unit. In this case, there is no skin incision. The trachea is punctured with a needle. This needle is used to pass a rigid guide on which are introduced larger and larger dilators until they reach the diameter of the cannula.
In extreme emergencies, a tracheostomy can also be performed under local anesthesia outside the operating room.
In which cases is a tracheostomy done?
Provisional tracheostomy is indicated in extreme urgency in cases of upper airway obstruction (asphyxia) when tracheal intubation is impossible or contraindicated.
A temporary tracheostomy can also be performed to prepare for laryngeal or pharyngeal surgery, to overcome difficult intubation during anesthesia, to allow prolonged mechanical ventilation in a person in intensive care.
A definitive tracheostomy can be done in people with advanced chronic respiratory failure, in case of central or peripheral anomaly of the oropharyngeal junction (mouth-pharynx) with swallowing disorders or in the event of neuromuscular diseases (such as myopathy) in which the weakening of the respiratory muscles or a defect in their control reduces the efficiency of breathing and requires ventilatory assistance.
After a tracheostomy
The consequences of this intervention are generally not considered painful. Analgesics administered after the operation relieve any pain. In the first few days, the cannula may be annoying or cause a reflex cough. It takes several days to get used to a tracheostomy tube and several weeks to not feel it at all. A tracheostomy does not prevent speaking or eating with some adjustments.
Living with a tracheostomy
When the tracheostomy is definitive (in the event of advanced chronic respiratory failure or in the event of neuromuscular disease, for example), the tracheotomy is experienced as a difficult stage. his physical integrity, the prospect of living with more constraint. However, it brings benefits. Breathing is more comfortable with this invasive ventilation than with non-invasive ventilation.
Health professionals teach tracheostomy patients and those around them what care is needed: change of cannula, care of the orifice of the trachea, endotracheal aspirations… They can train those around them to carry out this care.
To know : When a tracheostomy is temporary, removal of the cannula allows the opening of the pharynx to close within days.