Contents
Thrombocytémie
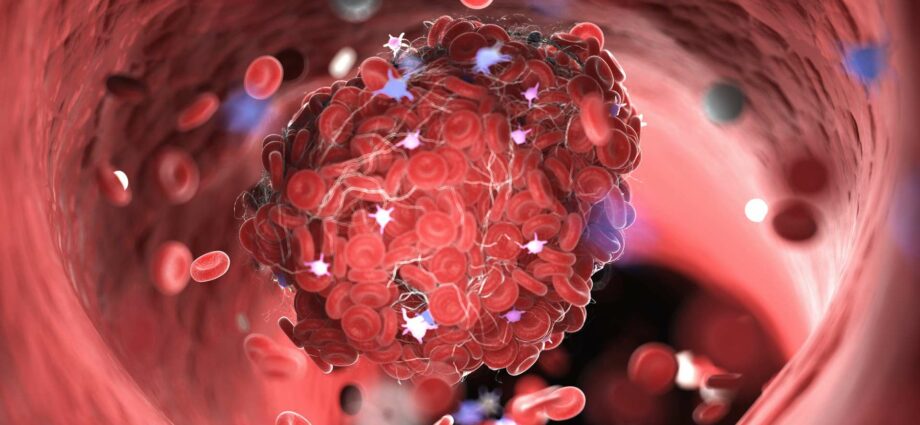
Thrombocythemia is a proliferation of blood platelets, with the consequence of an increased risk of thrombosis (blood clots). It is identified by blood sample or bone marrow biopsy. It is treated with aspirins or anti-platelets.
Thrombocythemia, what is it?
Definition
Thrombocythemia is a group of blood diseases. They mainly concern blood platelets, cells produced by the bone marrow and whose role is to clot the blood (make it more solid).
During a thrombocythemia the production of stem cells in the bone marrow is abnormal, it leads to the proliferation of blood platelet cells. However, their role being the coagulation of the blood, this proliferation leads to an increased risk of obstruction of the blood vessels: thrombosis.
To a lesser extent, thrombocythemia may result in bleeding without apparent injury.
Risks to the patient
It is especially the consequence of thrombocythemia that is to be feared. Thrombosis remains a major cause of mortality. The average survival of a person with untreated thrombocythemia is 12 to 15 years, but varies drastically depending on the extent of the thrombosis.
The other big consequence is the appearance of hemorrhages, (especially on the skin or in the mucous membranes). Thrombocythemia can cause nosebleeds, gums, bruising from small bumps, or even blood in the urine.
Causes of thrombocythemia
There are two types of thrombocythemia:
- Reactions, which are in reaction to a cloudiness. This disorder can take different forms, such as infection, inflammation, severe stress, lack of iron in the blood, or a tumor.
- The essentials, in 10 to 20% of cases, which appear without an established origin. They are part of the myeloproliferative syndromes.
Diagnose it
The diagnosis of thrombocythemia is made by blood sample. The threshold is evaluated at a platelet level greater than 450 per microliter, accompanied by normal parameters. This diagnosis can therefore be made simply by a routine blood test during a blood donation or medical examination.
Genetic testing can then be done to show the disease.
Sometimes a bone marrow biopsy (sample collection) is needed to test for stem cell production.
Risk factors
Thrombocythemia mainly affects adults between the ages of 50 and 70, as well as young women. Patients over 60 years of age may be at increased risk if they have a history of thrombosis (blood clots) or other blood accidents. However, a high platelet count is not an indicator of risk.
Recognize the symptoms of thrombocythemia
There is no truly characteristic symptom of thrombocythemia, but several clues stand out:
- Feeling of burning, redness, tingling at the extremities of the body (hands, feet), or conversely having cold fingertips.
- Pain in the chest
- Appearance of spots on vision
- Weakness of the body, dizziness
- Headaches
- Bleeding (frequent bruising, bleeding nose, sensitive gums)
The most effective way is to monitor your blood platelet count during routine examinations. It is estimated that half of thrombocythemia is detected without the patient even complaining of symptoms.
Treatment of thrombocythemia
Aspirin
Most cases of thrombocythemia are treated with aspirin, for its anti-coagulant properties, to reduce the risk of thrombosis, as well as to relieve symptoms.
Anti-platelets
Medicines such as hydroxyurea and anagrelides or interferon-alpha are taken until the blood platelet count returns to normal.
Thrombacytaphérèse
In an emergency, for example if the platelet count is too high, thrombacytapheresis can be performed. The purpose of the operation is to extract the patient’s blood, to remove the blood platelets before reinjecting it without its platelets.
The most severe cases may also be accompanied by a stem cell transplant for a young person.
As the disease is incurable in many cases, you will need to get used to taking this type of anti-coagulant medication regularly for the rest of your life.
Prevent thrombocythemia
Unlike reactive thrombocythemia, which appears following another disease, the essentials have an origin that is still very difficult to understand, and therefore no truly effective prevention.










Би цусны хорт хавдарын эм уугаад 10 жил болж байна. Он гарснаас хойш ойр ойрхон нилээн өвдлөө. Эмээ уугаад байгаа хэрнээ л байнга толгой өвдөж, зүрх дэлсэж, шөнөдөө хамаг бие өвдөөд байгаа. Энийг яаж шийдэхээ ч мэдэхгүй байна. Боломжтой бол зөвлөгөө өгөөч