Antibiotic-resistant bacteria are on the rise. Humanity itself is to blame for this, which invented antibiotics and began to use them widely, often even without the need. The bacteria had no choice but to adapt. Another victory of nature – the appearance of the NDM-1 gene – threatens to become final. What to do with it?
People do very often use antibiotics for the most trifling reason (and sometimes for no reason at all). This is how multidrug-resistant infections appear, which are practically not treated with antibiotics known to modern medicine. Antibiotics are useless in treating viral diseases because they simply do not work on viruses. But they act on bacteria, which in some quantity are always present in the human body. However, in fairness, it must be said that the “correct” treatment of bacterial diseases with antibiotics, of course, also contributes to their adaptation to unfavorable environmental conditions.
As the Guardian writes, “The age of antibiotics is coming to an end. Someday we will consider that two generations free from infections was just a wonderful time for medicine. So far the bacteria haven’t been able to strike back. It would seem that the end of the history of infectious diseases is so close. But now on the agenda is a “post-antibiotic” apocalypse.”
The mass production of antimicrobials in the mid-twentieth century ushered in a new era in medicine. The first antibiotic, penicillin, was discovered by Alexander Fleming in 1928. The scientist isolated it from a strain of fungus Penicillium notatum, the growth of which next to other bacteria had an overwhelming effect on them. Mass production of the drug was established by the end of World War II and managed to save many lives, which claimed bacterial infections that affected wounded soldiers after surgical operations. After the war, the pharmaceutical industry was actively engaged in the development and production of new types of antibiotics, more and more effective and acting on an ever wider range of dangerous microorganisms. However, it was soon discovered that antibiotics cannot be a universal remedy for bacterial infections, simply because the number of types of pathogenic bacteria is exceptionally large and some of them are able to resist the effects of drugs. But the main thing is that bacteria are able to mutate and develop means of combating antibiotics.
Compared with other living beings, in terms of evolution, bacteria have one indisputable advantage – each individual bacterium does not live long, and together they multiply rapidly, which means that the process of appearance and consolidation of a “favorable” mutation takes them much less time than, suppose a person. The emergence of drug resistance, that is, a decrease in the effectiveness of the use of antibiotics, doctors have noticed for a long time. Particularly indicative was the emergence of first resistant to specific drugs, and then multidrug-resistant strains of tuberculosis. World statistics show that about 7% of TB patients are infected with this type of tuberculosis. The evolution of Mycobacterium tuberculosis, however, did not stop there – and a strain with broad drug resistance appeared, which is practically not amenable to treatment. Tuberculosis is an infection with high virulence, and therefore the appearance of its super-resistant variety was recognized by the World Health Organization as especially dangerous and taken under special control of the UN.
The “end of the antibiotic era” announced by the Guardian is not the media’s usual tendency to panic. The problem was identified by English professor Tim Walsh, whose article “The Emergence of New Mechanisms of Antibiotic Resistance in India, Pakistan and the UK: Molecular, Biological and Epidemiological Aspects” was published on August 11, 2010 in the prestigious journal Lancet Infectious Diseases. The article by Walsh and his colleagues is devoted to the study of the NDM-1 gene, discovered by Walsh in September 2009. This gene, isolated for the first time from bacterial cultures obtained from patients who traveled from England to India and ended up on the operating table there, is extremely easy to transfer between different types of bacteria as a result of the so-called horizontal gene transfer. In particular, Walsh described such a transfer between the extremely common Escherichia coli E. coli and Klebsiella pneumoniae, one of the causative agents of pneumonia. The main feature of NDM-1 is that it makes bacteria resistant to almost all the most powerful and modern antibiotics such as carbapenems. Walsh’s new study shows that bacteria with these genes are already fairly common in India. Infection occurs during surgical operations. According to Walsh, the appearance of such a gene in bacteria is extremely dangerous, since there are simply no antibiotics against intestinal bacteria with such a gene. Medicine appears to have about 10 more years until the genetic mutation becomes more widespread.
This is not too much, given that the development of a new antibiotic, its clinical trials and the launch of mass production take a very long time. At the same time, the pharmaceutical industry still needs to be convinced that it is time to act. Oddly enough, the pharmaceutical industry is not too interested in the production of new antibiotics. The World Health Organization even states with bitterness that it is simply unprofitable for the pharmaceutical industry to produce antimicrobials. Infections usually heal too quickly: a typical course of antibiotics lasts no more than a few days. Compare with heart medications that take months or even years. And if not too much is needed for the mass production of the drug, then the profit turns out to be less, and the desire of corporations to invest in scientific developments in this direction also becomes less. In addition, many infectious diseases are too exotic, especially parasitic and tropical diseases, and are found far from the West, which can pay for medicines.
In addition to economic ones, there are also natural limitations – most new antimicrobial drugs are obtained as variants of old ones, and therefore bacteria “get used” to them quite quickly. The discovery of a fundamentally new type of antibiotics in recent years does not happen very often. Of course, in addition to antibiotics, healthcare is also developing other means to treat infections – bacteriophages, antimicrobial peptides, probiotics. But their effectiveness is still quite low. In any case, there is nothing to replace antibiotics for the prevention of bacterial infections after surgery. Transplantation operations are also indispensable: the temporary suppression of the immune system necessary for organ transplantation requires the use of antibiotics to insure the patient against the development of infections. Similarly, antibiotics are used during cancer chemotherapy. The absence of such protection would make all these treatments, if not useless, then extremely risky.
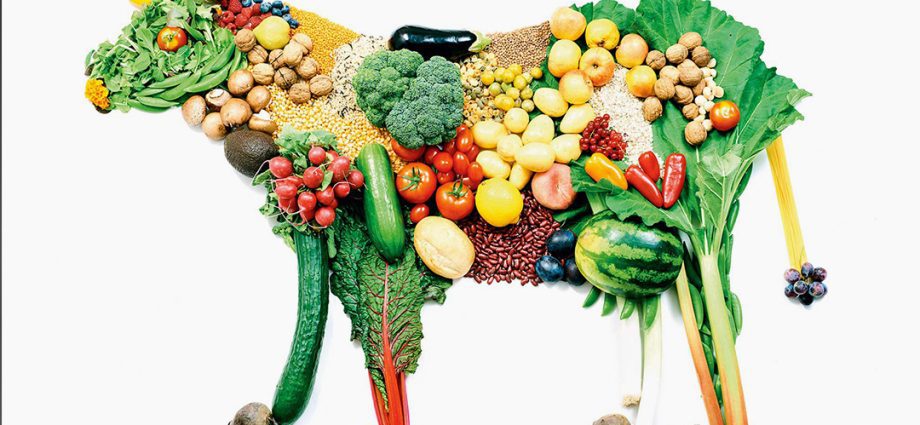
While scientists are looking for funds from a new threat (and at the same time money to fund drug resistance research), what should we all do? Use antibiotics more carefully and carefully: each use of them gives the “enemy”, bacteria, a chance to find ways to resist. But the main thing is to remember that the best fight (from the point of view of various concepts of healthy and natural nutrition, traditional medicine – the same Ayurveda, as well as simply from the standpoint of common sense) is prevention. The best way to fight infections is to constantly work on strengthening your own body, bringing it into a state of harmony.