Contents
Teratospermia: definition, causes, symptoms and treatment
Teratospermia (or teratozoospermia) is a sperm abnormality characterized by spermatozoa with morphological defects. As a result of these deformities, the fertilizing power of the sperm is impaired, and the couple may have difficulty conceiving.
What is teratospermia?
Teratospermia is a sperm abnormality characterized by sperm with morphologic defects. These abnormalities can affect different parts of the sperm:
- the head, which contains the nucleus carrying the 23 paternal chromosomes;
- the acrosome, a small membrane at the front of the head that, at the time of fertilization, will release enzymes that will allow the sperm to cross the pellucid area of the oocyte;
- the flagellum, this “tail” which allows it to be mobile and therefore to move up from the vagina to the uterus and then the tubes, for a possible encounter with the oocyte;
- the intermediate part between the flagellum and the head.
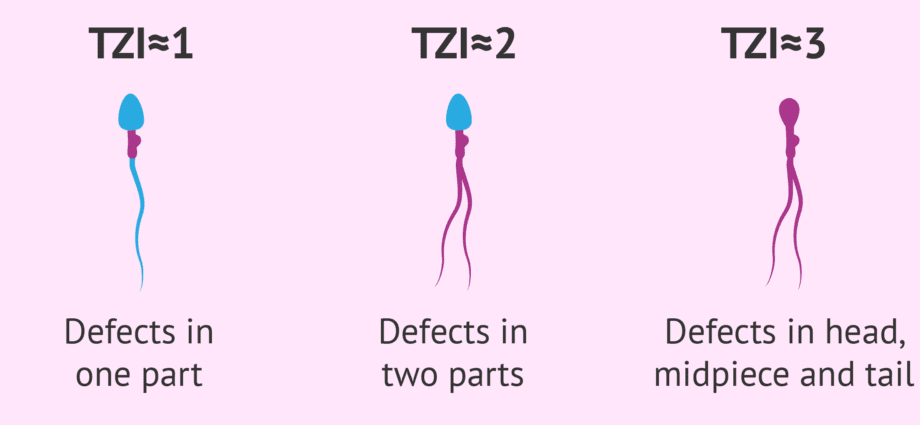
Often, the anomalies are polymorphic: they can be multiple, in size or shape, affect both the head and the flagellum, vary from one sperm to another. It can be globozoospermia (absence of acrosome), double flagellum or double head, coiled flagellum, etc.
All these anomalies have an impact on the fertilizing power of the sperm, and therefore on the fertility of the man. The impact will be more or less important depending on the percentage of normal sperm remaining. Teratospermia can decrease the chances of conception, and even lead to male infertility if it is severe.
Often, teratospermia is associated with other spermatic abnormalities: oligospermia (insufficient number of spermatozoa-, asthenospermia (defect in sperm mobility. This is called oligo-astheno-teraozoospermia (OATS).
The causes
Like all sperm abnormalities, the causes can be hormonal, infectious, toxic, or medicinal. The morphology of spermatozoa is in fact the first parameter to be altered by an external factor (exposure to toxins, infection, etc.). More and more specialists consider that atmospheric and food pollution (via pesticides in particular) has a direct impact on the morphology of spermatozoa.
But sometimes, no cause is found.
Symptoms
The main symptom of teratospermia is difficulty conceiving. The fact that the shape of the sperm is abnormal does not affect the occurrence of malformations in the unborn child, but only the chances of pregnancy.
The diagnosis
Teratospermia is diagnosed using a spermogram, one of the first examinations systematically performed in men during an infertility assessment. It allows a qualitative and quantitative study of the sperm thanks to the analysis of different biological parameters:
- the volume of the ejaculate;
- the pH;
- sperm concentration;
- sperm mobility;
- sperm morphology;
- sperm vitality.
The part about sperm morphology is the longest and most difficult part of the spermogram. In a test called a spermocytogram, 200 sperm are fixed and stained on smear slides. Then the biologist will study the different parts of the sperm under a microscope in order to assess the percentage of morphologically normal sperm.
The type of morphological abnormalities is also taken into account to estimate the impact of teratospermia on fertility. Several classifications exist:
- the David classification modified by Auger and Eustache, still used by certain French laboratories;
- the Kruger classification, the WHO international classification, is the most widely used in the world. Carried out using an automatic machine, this more “severe” classification classifies as atypical spermatozoa any spermatozoon which deviates, even very little, from the form considered to be normal.
If the proportion of properly formed sperm is less than 4% according to the WHO classification, or 15% according to the modified David classification, teratospermia is suspected. But as for any spermatic abnormality, a second or even a third spermogram will be carried out 3 months apart (the duration of a spermatogenesis cycle being 74 days) in order to make a firm diagnosis, especially as different factors can influence on sperm morphology (long abstinence time, regular cannabis intake, feverish episode, etc.).
A migration-survival test (TMS) usually completes the diagnosis. It makes it possible to have an evaluation of the number of spermatozoa capable of ending up in the uterus and capable of fertilizing the oocyte.
A sperm culture is often coupled with the spermogram in order to detect an infection which could alter spermatogenesis and lead to morphological defects of the sperm.
Treatment for having a child
If an infection is found during the sperm culture, antibiotic treatment will be prescribed. If exposure to certain toxins (tobacco, drugs, alcohol, medication) is suspected to be the cause of teratospermia, elimination of the toxins will be the first step in management.
But sometimes no cause is found and the use of ART will be offered to the couple. The percentage of spermatozoon of normal form being a good indicator of the natural fertilizing capacity of the spermatozoon, it constitutes an element of decision, with in particular the migration-survival test, in the choice of the technique of ART: intra- insemination. uterine (IUI), in vitro fertilization (IVF) or in vitro fertilization with intracytoplasmic injection (IVF-ICSI).