Contents
Symptoms, causes and treatments of jaundice
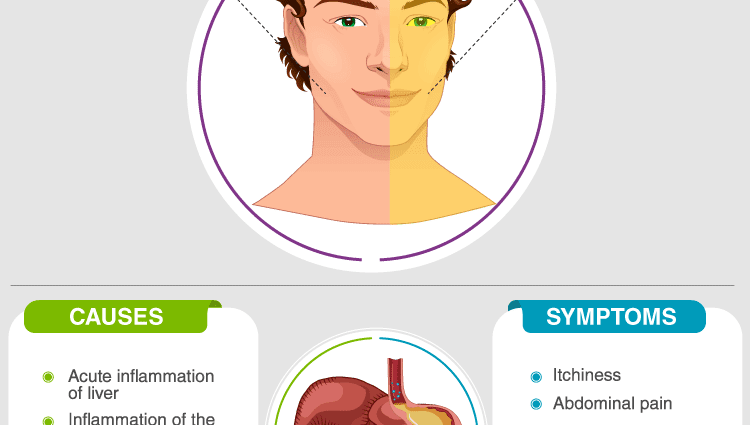
Symptoms of jaundice
Apart from its aesthetic consequences, the change in color of the integuments (skin and mucous membranes) has no pathological consequences. Depending on the causes of jaundice, other signs may be associated, possibly making it possible to orient the diagnosis: abdominal pain, fever, itching, fatigue, joint pain, etc.
Free bilirubin, therefore not yet “conjugated” in the liver, is toxic to the brain. In newborns, its accumulation in too large a quantity can be particularly harmful for the brain and require urgent treatment.
What are the causes ?
Apart from the toxicity of free bilirubin for the brain (neurotoxicity), in the vast majority of cases, the causes of jaundice determine the prognosis, benign or severe depending on the case. Likewise, treatment differs depending on the origin of the jaundice. The exact diagnosis is therefore essential. To make this diagnosis, doctors use first-line clinical examination, a blood test and ultrasound of the abdomen. Other explorations may then be necessary: CT scan, MRI, cholangiography, endoscopy, biopsy, etc.
Since jaundice is a symptom and not a disease, it is not contagious.
Basically, there are two different kinds of jaundice:
- It may be an increased production of free bilirubin
- Or it can be conjugated bilirubin.
In the first case, during an increase in free bilirubin, the excess may be related to an increased destruction of red blood cells (hemolysis) or a poor conjugation of bilirubin in the liver. The first situation often causes anemia (drop in hemoglobin level) and can suggest a blood disease, or an infection, a drug cause, immunological damage, etc.
In the case of jaundice due to an increase in conjugated bilirubin, the jaundice is most often related to a genetic disease (Gilbert’s disease) causing insufficient conjugation of bilirubin. This Gilbert’s disease or Gilbert’s syndrome is benign in the vast majority of cases.
In the second case, when it is an excess of conjugated bilirubin, there is increased elimination in the urine which takes on a darker color associated with discoloration of the stools. Two types of causes can be suspected. First, liver damage (hepatitis, cirrhosis, parasitosis, etc.) or an obstacle on the bile ducts here preventing the elimination of bilirubin. In this latter case, we are especially looking for a calculation, blocking the passage, for a local tumor compressing the bile ducts… Other rarer hepato-biliary causes can also be responsible for jaundice.
The special case of jaundice in babies
In the newborn child, there are several causes of jaundice that are specific to this period of life.
The liver is sometimes not mature enough to conjugate bilirubin. However, the latter increases greatly because the newborn must “exchange” his fetal hemoglobin for an adult form, which causes the destruction of many red blood cells in a very short time, a phenomenon which can be the cause of jaundice.
Jaundice in mother’s milk can also be seen in breast-fed infants.
A blood incompatibility between the fetus and its mother can be responsible for the destruction of red blood cells and therefore for a strong accumulation of bilirubin. This is the case when the mother is Rh negative and her child is Rh positive. The mother then becomes immune to the Rhesus factor in her fetus and makes antibodies that pass through the placenta to destroy the baby’s red blood cells. As long as the child is not born, bilirubin is eliminated by the placenta, but, after childbirth, its accumulation causes jaundice.
Apart from other causes related to congenital diseases, significant hematomas that can occur during childbirth can also release a lot of hemoglobin and therefore ultimately bilirubin.
Treatments for jaundice
Prevention of jaundice is not possible in all cases. Nevertheless, precautions allow certain causes to be limited.
Here are the measures that can prevent the onset of diseases that can lead to jaundice:
- Moderate moderate alcohol consumption,
- Get vaccinated against hepatitis B or A,
- Have safe sex,
- Respect hygiene rules in countries at risk of infectious transmission by Food,
- Avoid fasting or dehydrating if you have Gilbert’s syndrome.
The treatment of jaundice is that of its cause:
- Sometimes no management is necessary: this is the case in hereditary Gilbert’s disease, which can cause flare-ups of jaundice usually not serious, especially during a period of fasting or dehydration.
- In other situations, the resolution of the cause leads to that of jaundice (hepatitis, resorption of hematomas, etc.).
- In mother’s milk jaundice, heating the latter to 60 ° C, or switching to formula, usually resolves the situation.
- In “physiological” jaundice of the newborn, exposure to blue light facilitates the elimination of bilirubin. Sometimes this measure is insufficient and, given the neurological risk, it is necessary to perform an exsanguino-transfusion (all the baby’s blood is changed and replaced with a transfusion). – In other cases, surgery is required (stones, tumors), or the administration of specific drugs (infections, blood diseases, cancer).