Contents
Splenectomy
Splenectomy is the surgical removal of the spleen. It is a frequent digestive operation, but more and more, alternatives are favored because of the possible complications of this intervention.
What is splenectomy?
Splenectomy refers to the surgical operation to remove the spleen.
As a reminder, the spleen is a very vascularized organ the size of a fist, located at the top left of the abdomen, just under the diaphragm and against the stomach. A secondary lymphatic organ, it is made up of three areas with different functions: the red pulp, the white pulp and the marginal area that separates them. One of the functions of the spleen is to store red blood cells and recycle them once their life cycle has ended. It also plays a key role in immunity via various mechanisms: its action of filtering the blood of the splenic artery eliminates certain pathogenic agents while some of its lymphocytes produce specific antibodies.
Splenectomy can be total (the spleen is completely removed) or partial. The patient will then be said to be asplenic (he no longer has a spleen at all) or hyposplenic (he only has part of it).
How does the splenectomy work?
Depending on its indication, splenectomy can be scheduled (elective) or performed urgently.
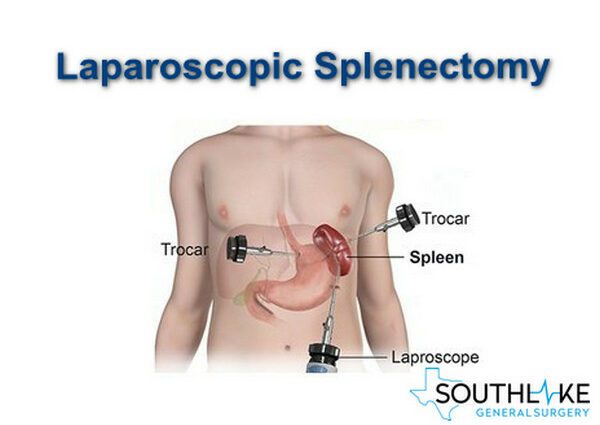
The operation is performed under general anesthesia, by laparoscopy (with small holes) or, if the volume of the spleen is too large or in case of intra-abdominal hemorrhage, by laparotomy, with an incision in the abdomen.
The surgeon begins by ligating and then cutting the artery and splenic vein that supply the spleen. He then proceeds to the total or partial ablation of the spleen. As the spleen is highly vascularized, its removal is an operation with a high risk of bleeding.
When to have a splenectomy?
Basically, there are two main indications for splenectomy: an underlying pathology and accidental rupture of the spleen.
The so-called elective splenectomy can be performed in the face of different pathologies:
- an autoimmune disease of the spleen, such as autoimmune hemolitic anemia;
- blood disorders: thalassemia, sickle cell anemia (sickle cell disease), idiopathic thrombocytopenic purpura (ITP);
- a genetic disease affecting the form of red blood cells, such as hereditary micro-spherocytosis (Minkowski-Chauffard disease);
- an enlarged spleen;
- cysts in the spleen (splenic cysts);
- a benign tumor of the spleen;
- certain leukemias or lymphomas affecting the spleen (hairy cell leukemia).
The surgeon may have to carry out an emergency splenectomy in the event of partial or total rupture of the spleen after a trauma (car accident, direct shock during sport, for example). This is called a hemostasis splenectomy, because its purpose is to stop the bleeding. The spleen being very vascularized and spongy, it is an organ which can indeed rupture under the effect of a shock, with the risk of causing a hemorrhage. Faced with a violent trauma on the abdomen and / or warning signs (paleness, increased heart rate, severe pain, hard and tense abdomen), an ultrasound, or even a CT scan, will be performed to confirm the diagnosis of rupture (total or partial) of the spleen. Given the high risk of complications after the operation, however, trauma surgery has become much more conservative, thanks in particular to the use of radiological embolization techniques.
Finally, in certain cases, splenectomy may be for diagnostic purposes.
After splenectomy
Operative suites
The length of stay depends on the surgical technique: it is about 7 days for a laparotomy, less for a laparoscopy. The patient can then go home with a sick leave of 1 month.
Risks and complications
The two major complications of splenectomy are the risk of infection and the risk of thromboembolism.
As the spleen is no longer there to perform its various immune roles, the risk is indeed increased for certain infections affecting red blood cells. These are mainly infections caused by so-called encapsulated bacteria, such as Streptoccocus pneumoniae, Haemophilus influenzae et Neisseria meningitidis. The most feared pathology is post-splenectomy septic syndrome or “Overwhelming Post Splenectomy Infection” (OPSI). To limit this risk, antibiotic treatment is prescribed for at least 2 years, and sometimes for life in certain patients at risk. In addition to the vaccines recommended in the immunization schedule, people with splenectomy should be vaccinated against influenza (annually), pneumococci, meningococci, and Haemophilus influenzae type b regardless of their age. In the event of travel to a country at risk or animal bites, certain precautions should be taken. Finally, the splenectomized patient must consult urgently in the face of any high fever.
The risk of thrombus is also increased in the event of splenectomy. The mechanism is however still unknown, and the risk seems to depend on the indication of the intervention. Platelets are regularly checked in the splenectomized patient.