Contents
Salpingitis: inflammation of the fallopian tubes
What is salpingitis?
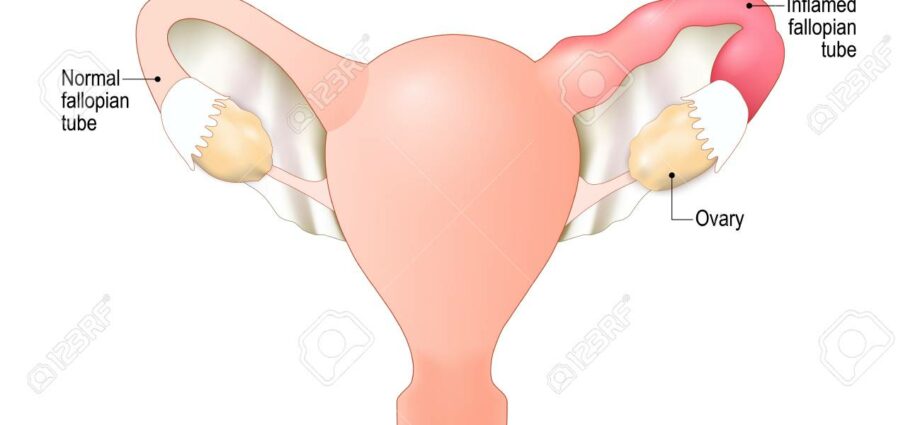
A salpingitis corresponds to a inflammation of uterine tubes, or fallopian tubes. Two in number, connecting the uterus to the ovaries, the uterine tubes are essential structures of the female reproductive system. In salpingitis, both fallopian tubes are usually affected.
What are the causes of salpingitis?
In the majority of cases, salpingitis is caused by sexually transmitted infection (STI) such as :
- la chlamydia, caused by the bacteria Chlamydia trachomatis, which accounts for about 60% of cases of salpingitis;
- la gonorrhea or “hot piss”, due to bacteria Neisseria gonorrhoeae, which represents between 5 and 10% of cases of salpingitis;
- a mycoplasma infection, which can be caused by Mycoplasma hominis et Ureaplasma urealyticum, which represents between 5 and 20% of cases of salpingitis.
While STIs are the most common causes of salpingitis, it can also be caused byother infectious agents including streptococci, staphylococci, enterococci and enterobacteriaceae. Infection with these germs can result from:
- another infection having taken place in an organ close to the genital tract;
- a surgical intervention such as uterine curettage and voluntary termination of pregnancy (abortion) by surgery;
- an endo-uterine medical examination such as hysterosalpingography and hysteroscopy;
- the insertion of an IUD, or intrauterine device (IUD).
In rare cases, salpingitis can also be the result of a specific infection such as tuberculosis or bilharzia.
Who is affected by salpingitis?
Between 55 and 70% of cases of salpingitis concern women under the age of 25. The people most at risk are young women who have not yet had children.
What is the risk of complications?
Acute salpingitis can progress gradually, become chronic and cause complications. In the most serious cases, this silent development can lead to sterility.
What are the symptoms of salpingitis?
In 50-70% of cases, acute salpingitis is asymptomatic, that is, it is invisible with the absence of characteristic symptoms. This makes it particularly difficult to diagnose the infection.
In other cases, salpingitis can present with different signs such as:
- a fever quite high, which may be accompanied by chills;
- pain in the lower abdomen, which can occur unilaterally or bilaterally, and which can also radiate down the thighs, down the back or even to the external genitalia;
- leucorrhoea, that is, non-bloody discharge from the vagina, which is profuse and yellowish, and in some cases purulent;
- metrorrhagia, which designate blood loss of uterine origin;
- urination burns;
- frequent urges to urinate;
- gastrointestinal disorders such as nausea, bloating or constipation.
What are the risk factors?
The risk of developing acute salpingitis is greater in the following cases:
- unprotected sex;
- multiple sexual partners;
- history of STIs or salpingitis;
- urethritis in the sexual partner;
- endo-uterine medical examinations;
- endo-uterine surgery.
How to treat salpingitis?
Salpingitis needs to be treated as soon as possible to limit the risk of complications, and particularly the risk of infertility. Hospitalization may be necessary.
The medical management of salpingitis is based on drug therapy and strict bed rest. Antibiotic therapy is put in place depending on the pathogenic germ responsible for the infection. Analgesics, antispasmodics and anti-inflammatory drugs can also be used depending on the case.
Drug treatment is accompanied by preventive measures:
- abstaining from sex or wearing condoms until healing is complete;
- screening and treatment of the partner (s);
- carrying out screening tests for different STIs.
To limit the risk of recurrence, medical surveillance is also instituted following the treatment of salpingitis.