Contents
Pheochromocytomas: understanding diseases of the adrenal medulla
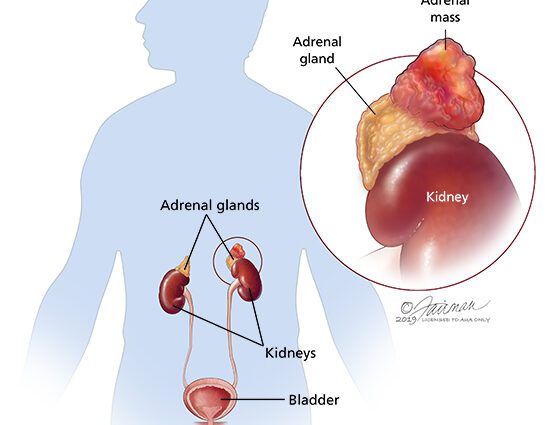
Pheochromocytoma is an adrenal tumor (gland located above the kidneys) which is generally benign. It causes persistent or paroxysmal hypertension. Imaging exams, including MRI or CT scan, help locate tumors. The treatment of this tumor is mainly based on surgery.
Definition of pheochromocytomas
Pheochromocytomas are rare tumors (less than 1 in 100) of the autonomic nervous system and are usually benign. About 000% of pheochromocytomas are located in the adrenal medulla (inner part of the adrenal capsules). As with other neuroendocrine tumors, malignancy is defined by the presence of distant metastases.
Pheochromocytomas are seen in men and women and are malignant in less than 10% of cases. Although pheochromocytomas are observed at any age, the peak incidence is between 20 and 50 years. Pheochromocytomas vary in size, on average 5 to 6 cm in diameter, and weigh from 50 to 200g. They are rarely large enough to be palpated.
What are the symptoms ?
Arterial hypertension, which is paroxysmal in 45% of patients, is the main sign. About 1/1000 of people with high blood pressure have pheochromocytoma. The symptoms consist of:
- tachycardia (rapid heartbeat), sweating, hypotension;
- tachypnea (rapid breathing), chest pain with angina, palpitations;
- severe headache (headache), nausea, vomiting;
- dypnea, feeling of impending catastrophe;
- cooling of the extremities, pallor;
- visual disturbances.
Paroxysmal seizures occur in half of those affected. seizures can be triggered by palpation of the tumor, by changes in position, abdominal compression or massage, induction of anesthesia. In the elderly patient, severe weight loss with persistent hypertension is suggestive of pheochromocytoma.
Pheochromocytomas can be very small. However, even a small pheochromocytoma can produce large amounts of catecholamines. Catecholamines are hormones like adrenaline, norepinephrine, and dopamine, which tend to dramatically increase blood pressure and heart rate and cause other symptoms usually associated with life-threatening situations.
Diagnostic
The diagnosis is based on the demonstration of excess catecholamines.
Several assays are possible, such as that of metabolites and catecholamines in the blood or urine. The best dosages seem to be the dosage of metanephrines and normetanephrines in 24-hour urine and plasma normetanephrines. To limit false positives (positive test when the patient is not really a carrier of the disease), it is recommended to perform the urine dosage in case of low suspicion of pheochromocytoma. Conversely, in the event of a strong suspicion of the disease, the plasma dosage is preferred.
Once the suspicion of pheochromocytoma is confirmed by biology, the tumor is localized by MRI and CT imaging of the chest and abdomen.
Treatment of pheochromocytomas
The standard treatment is surgery. The latter should always be performed after premedication to normalize blood pressure and slow heart rate to avoid preoperative complications. Usually alpha-adrenergic blockers are the drug treatment of choice.
The surgery consists of laparoscopy (endoscopy and not opening the abdomen), for intrasadrenal pheochromocytomas. This route reduces postoperative pain, the risk of bleeding and the number of days in hospital compared to open surgery by laparotomy (opening of the abdomen).
Postoperatively, during the first 24-48 hours, it is important to monitor the patient’s blood pressure, heart rate and blood sugar levels in order to reduce postoperative complications which are mainly hypotension, hypertension as well as hypoglycaemia.
Because of a risk of malignancy which is not zero, patients must have a biological follow-up at three months and then annually. In the case of a new elevation, one should look for metastases by new imaging. Follow-up should be done for at least 10 years. The treatment of these metastatic forms requires a multidisciplinary team (oncologist, nuclear doctor, endocrinologist and surgeon).