Contents
Ostéomalacie
What is it ?
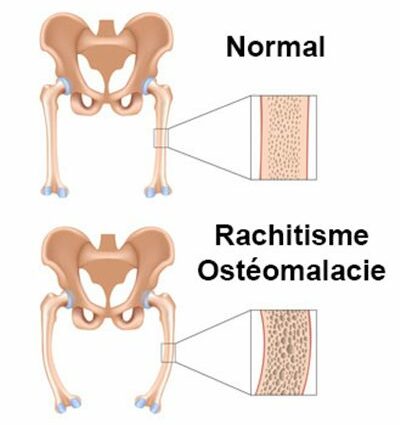
Osteomalacia is generalized osteopathy (bone pathology). This affection is the consequence of a deficient primary mineralization of the bone matrix making the bone “soft” and being able to generate its deformation. In the case of osteomalacia, the bone mass is normal but the mineralization of the osteoid tissue is deficient, a consequence of an accumulation of osteoblasts (cells secreting the bone matrix). Osteomalacia is different from osteoporosis in which bone mass is deficient but bone mineralization is normal.
The bone structure is the generic term defining the “organic” substance on which a “mineral” substance is fixed. This mineral substance is characterized by a mixture of calcium and phosphorus. These minerals give bone its hardness and strength. (5)
In the case of osteomalacia, this bone structure is therefore of normal density. The problem results from insufficient fixation of calcium crystals on this bone framework. Several cases can explain this calcium insufficiency:
(1) Calcium uptake is promoted by a supply of vitamin D. This vitamin is involved in the absorption and metabolism of calcium. A deficient intake of Vitamin D can therefore be the cause of insufficient fixation of calcium on the bone structure.
(2) The regulation of calcium levels in the blood is regulated, among other things, by a hormone secreted by the parathyroid glands (located in the neck): parathyroid hormone. An excess of this hormone can also disrupt the fixation of the mineral in the bone matrix.
(3) Daily calcium intake by the diet is diverse according to the age and physiological state of the person:
– Between 4 to 8 years old: 800 mg / day
– Between 9 and 18 years old: 1 mg / day
– Between 19 and 50 years old: 1 mg / day
– Between 50 years and over: 1 mg / day
– For pregnant and breastfeeding women: 1 mg / day
A lower calcium intake compared to the daily recommendations can lead to calcium deficiency in the person and thus lead to deficient bone mineralization. (4)
The bone therefore becomes more ductile due to this mineral insufficiency at the level of the bone framework. Certain bones in the body support greater loads (vertebrae, legs). These then run the risk of deforming or even cracking.
In children, osteomalacia is synonymous with rickets.
Symptoms
Symptoms specific to osteomalacia are mainly pain in the bones. These pains can be localized in the legs (accentuated during walking, running, etc.), spine, ribs, shoulder blades, pelvis, and others.
This rheumatism is essentially non-specific and quite diffuse.
To these pains, can be added more or less visible deformations or even by mechanical characteristics: waddling gait, proximal myopathy (pathology affecting the muscle fibers), muscle weakness, etc.
In the case of severe forms, osteomalacia can be characterized by a “bell-shaped” or “violin” thorax, a keel-shaped sternum or even a loss of size.
Calcium is also an essential mineral salt in the formation of dentition. In addition to bone symptoms, abnormalities in the dental enamel (loss of shine of the teeth and weakening of the teeth) may appear. (1)
The origins of the disease
Osteomalacia is due to a calcium defect in the bone structure. These two conditions are due to a deficiency in vitamin D or / and calcium, coming from the diet (or from exposure to natural sunlight for Vitamin D).
Rickets affects growing children whose bones are still forming.
Osteomalacia, on the other hand, affects adults (more women and the elderly) whose bone mass is well formed. (2)
Risk factors
Osteomalacia is a pathology that mainly affects women and the elderly.
Nevertheless, certain factors can be at the origin of an increased risk of the development of this pathology such as the taking of anticonvulsant drugs, cancers, phosphate, vitamin D, insufficient exposure to the sun, a family history of disorders of the vitamin D metabolism, kidney failure, some liver disease, etc.
Children whose vitamin D and calcium intake are insufficient may also be affected by this type of pathology in the form of rickets.
Prevention and treatment
An early diagnosis of this pathology makes it possible to limit the consequences.
After consultation with the doctor, this one can prescribe a phosphocalcic balance to you in order to evaluate the deficiencies in calcium, phosphorus and albumin. This assessment can be supplemented by a determination of calcium in the urine (calciuria).
These checks may be accompanied by x-rays of the painful bones. The presence of a slightly dirty opaque appearance and Looser-Milkman streaks (characteristic of this rheumatism) can be significant of osteomalacia. (5)
In addition, computed tomography of the spine makes it possible to study the structure of the vertebrae.
Finally, it is also possible to perform a bone biopsy in order to find demineralized bone tissue and increased osteoblast activity.
The treatment of osteomalacia is primarily preventive.
A recommended daily intake of calcium helps to avoid any mineral calcium deficit. This daily intake is made through food (mainly in dairy products, fish and fortified soy drinks) but also through certain mineral waters rich in calcium and easy to absorb.
Vitamin D is also involved in the prevention of this pathology. Vitamin D is found in food (also present in milk, fatty fish such as salmon or trout, eggs, liver, etc.). Vitamin D intake is also possible through moderate exposure to the sun helping the body to biologically design this vitamin.
The curative treatment of the disease consists of the administration of concentrated Vitamin D. Usually accompanied by additional calcium intake.
Increased exposure (but not excess) to the sun is often advised for people with osteomalacia. (3)
A well-conducted treatment leads to a rather rapid recovery with a reduction or even a disappearance of pain. (3)