Contents
Menstrual cycle: the follicular phase
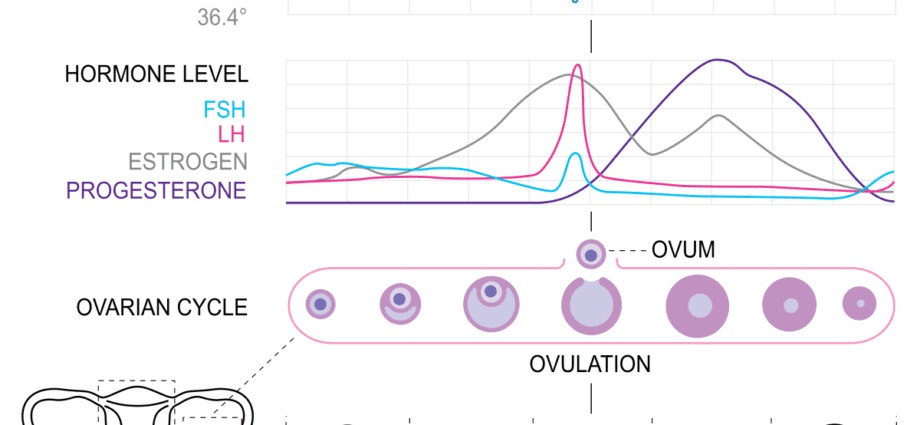
From puberty to menopause, the ovaries are the site of periodic activity. The first stage of this menstrual cycle, the follicular phase corresponds to the maturation of an ovarian follicle which, at the time of ovulation, will release an oocyte ready to be fertilized. Two hormones, LH and FSH, are essential for this follicular phase.
The follicular phase, the first phase of the hormonal cycle
Each little girl is born with, in the ovaries, a stock of several hundred thousand so-called primordial follicles, each containing an oocyte. Every 28 days or so, from puberty to menopause, an ovarian cycle takes place with the release of an oocyte – ovulation – by one of the two ovaries.
This menstrual cycle is made up of 3 distinct phases:
- the follicular phase;
- l’ovulation ;
- the luteal phase, or post-ovulatory phase.
The follicular phase begins on the first day of menstruation and ends at the time of ovulation, and therefore lasts an average of 14 days (over a 28-day cycle). It corresponds to the follicular maturation phase, during which a certain number of primordial follicles will be activated and begin their maturation. This folliculogenesis includes two main stages:
- the initial recruitment of follicles: a certain number of primordial follicles (some 25 thousandths of a millimeter in diameter) will mature until the stage of tertiary follicles (or anthrax);
- the growth of the antral follicles to the pre-ovulatory follicle: one of the antral follicles will detach from the cohort and continue to mature, while the others are eliminated. This so-called dominant follicle will reach the stage of pre-ovulatory follicle, or De Graaf follicle which, during ovulation, will release an oocyte.
Symptoms of the follicular phase
During the follicle phase, the woman does not feel any particular symptoms, apart from the onset of menstruation which signals the start of a new ovarian cycle and therefore the start of the follicular phase.
Production of estrogen, FSH and LH hormones
The “conductors” of this ovarian cycle are different hormones secreted by the hypothalamus and pituitary gland, two glands located at the base of the brain.
- the hypothalamus secretes a neurohormone, GnRH (gonadotropin releasing hormone) also called LH-RH, which will stimulate the pituitary gland;
- in response, the pituitary gland secretes FSH, or follicular stimulating hormone, which will activate a certain number of primordial follicles which then enter into growth;
- these follicles in turn secrete estrogen which will thicken the uterine lining in order to prepare the uterus to receive a possible fertilized egg;
- when the dominant pre-ovulatory follicle is selected, estrogen secretion increases sharply, causing a surge in LH (luteinizing hormone). Under the effect of LH, the tension of the fluid inside the follicle increases. The follicle eventually breaks and releases its oocyte. It’s ovulation.
Without follicular phase, no ovulation
Without a follicular phase, there is indeed no ovulation. This is called anovulation (absence of ovulation) or dysovulation (ovulation disorders), both of which result in the absence of production of a fertilizable oocyte, and therefore infertility. Several causes can be at the origin:
- a problem with the pituitary or hypothalamus (hypogonadism of “high” origin), which causes an absent or insufficient hormonal secretion. Excessive secretion of prolactin (hyperprolactinemia) is a common cause of this dysfunction. It can be due to a pituitary adenoma (a benign tumor of the pituitary gland), to the taking of certain drugs (neuroleptics, antidepressants, morphine…) or certain general diseases (chronic renal failure, hyperthyroidism,…). Significant stress, emotional shock, significant weight loss can also interfere with the proper functioning of this hypathalamic-pituitary axis and lead to transient anovulation;
- Polycystic ovary syndrome (PCOS), or ovarian dystrophy, is a common cause of ovulation disorders. Due to hormonal dysfunction, an abnormal number of follicles accumulates and none of them come to full maturation.
- ovarian dysfunction (or hypogonadism of “low” origin) congenital (due to a chromosomal abnormality, Turner syndrome for example) or acquired (following chemotherapy treatment or surgery);
- early menopause, with the premature aging of the oocyte reserve. Genetic or immune causes could be at the origin of this phenomenon.
Ovarian stimulation during the follicular phase
In the presence of anovulation or dysovulation, treatment for ovarian stimulation may be offered to the patient. This treatment consists of stimulating the growth of one or more follicles. Different protocols exist. Some resort to clomiphene citrate, an antiestrogen taken by mouth that tricks the brain into thinking the estradiol level is too low, causing it to secrete FSH in order to stimulate the follicles. Others use gonadotropins, injectable preparations containing FSH and / or LH that will support the maturation of follicles. In both cases, throughout the protocol, the patient is regularly followed with monitoring including blood tests to measure hormone levels and ultrasound scans to control the number and growth of follicles. Once these follicles are ready, ovulation is triggered by an injection of HCG.