Contents
Medical treatments for rheumatoid arthritis (rheumatism, arthritis)
Many progress have been made in recent years for the relief and control of rheumatoid arthritis. Research has shown that treatment with anti-rheumatic drugs during the first 3 to 6 months of the disease increases the chances of remission prolonged. Often the same treatments help control the disease and prevent its progression. Therefore, these drugs are an essential part of treatment.
The goals processing are as follows:
- relieve symptoms;
- attempt to induce and maintain remission of the disease;
- restore or maintain the proper functioning of the joints;
- prevent disability and disease damage on other organs.
What do we mean by “remission”? – The absence of symptoms of inflammation, such as morning stiffness and pain; – The absence of signs of inflammation on physical examination, in the joints and elsewhere in the body; – The absence of signs of inflammation in the blood, in blood tests; – A halt in the progression of joint damage, visible on x-ray. |
pharmaceuticals
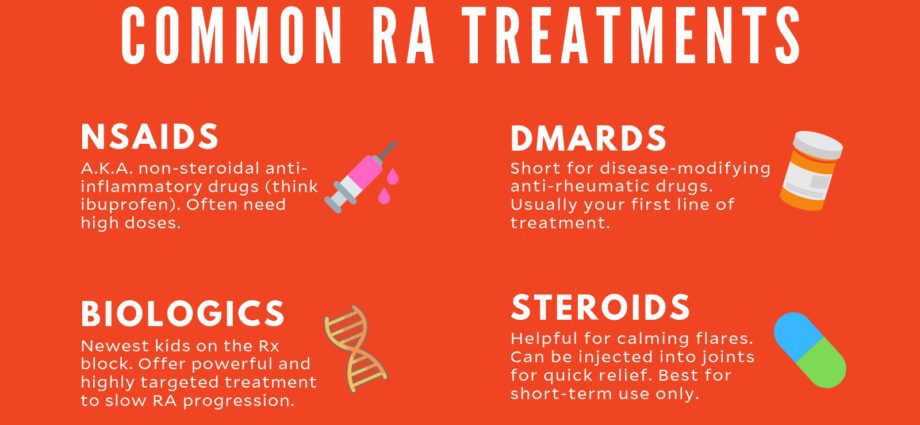
Two types of pharmaceuticals are generally used for the treatment of rheumatoid arthritis: symptomatic or symptomatic medicines relief (nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids) and DMARDS. These are intended to prevent flare-ups and control symptoms over a long period of time. They include classic treatments (such as immunosuppressants) and biotherapies or biological response modifiers.
Symptomatic (relieving) drugs
Anti-inflammatory drugs reduce pain and stiffness in the joints. They do not slow down the progression of the disease and do not prevent the occurrence of possible joint deformities. They are mainly used at the beginning of the disease, and then intermittently, in the event of pain in order to relieve. It is recommended to use them in combination with a basic treatment, in order to slow down the progression of the disease.
- Classic nonsteroidal anti-inflammatory drugs (NSAIDs). Ibuprofen (eg, Advil® and Motrin®), naproxen (eg, Anaprox® and Naxen®), and all other anti-inflammatory drugs are helpful in relieving symptoms. Aspirin (acetylsalicylic acid) is little used because it is less well tolerated by the digestive system.
Side effects. Regular use of conventional nonsteroidal anti-inflammatory drugs may be associated with gastrointestinal disturbances, such as heartburn, ulcers or sometimes severe digestive bleeding, as well as others side effects such as high blood pressure or kidney failure. They are therefore used for the shortest possible time, only as needed. They are sometimes combined with a medicine to protect the stomach, such as omeprazole (Mopral®), or misoprostol (Cytotec®).
Anti-inflammatory drugs can have significant side effects, especially cardiovascular, with an increased risk of heart attack or stroke. These treatments must therefore be followed very closely by the doctor. One worrying aspect is that these complications can occur quickly, in some cases within the first week. Even brief use therefore presents a certain risk.
The NSAIDs presenting the least risk would be naproxen and ibuprofen (low dose); the risk would be low to zero. It is therefore clear that one should not take these drugs lightly. |
- Corticosteroids. Corticosteroids (cortisone, prednisone, prednisolone) are very effective drugs for reducing inflammation and relieving joint pain and stiffness. They may also delay the progression of rheumatoid arthritis, especially when used in combination with a DMARD 37. These drugs are taken as tablets or injected directly into the joints. They are often prescribed at the onset of the disease, but their long-term use is limited by the significant unwanted side effects. Their anti-inflammatory action is rapid, but short-lived. The doctor always suggests the lowest effective dose for the shortest time possible in order to limit side effects.
Side effects. In the long term, corticosteroids can cause serious side effects, sometimes even very serious ones. These vary depending on the dose taken. For example: weight gain, increased risk of osteoporosis, high blood pressure and infections …
Intra-articular corticosteroid injections or infiltrations. They are very effective in the event of a crisis, especially if the number of affected joints is not too high. However, it should not be abused, as repeated injections of corticosteroids into the joints can damage the joints and / or cause the same side effects as if taken orally. In general, doctors limit themselves to 3 or 4 injections per joint per year. |
- Ofacetaminophen (paracetamol) to morphine derivatives are sometimes used to reduce pain when it is severe.
Long-term anti-rheumatic drugs
Anti-rheumatic drugs are prescribed when symptoms persist for several weeks. They act directly on the disease by fighting immune cells that attack the joints. This gives them the ability to prevent or delay joint damage. These drugs (many of which are immunosuppressants) are even more beneficial if taken early in the disease. They are fully effective after a few weeks to a few months. They can be combined with NSAIDs or corticosteroids without any problem.
In this category of drugs, the methotrexate (Novatrex®), is most frequently used as a first-line treatment, in the form of tablets or subcutaneous injections. It is recommended that people taking this medicine take folic acid supplements to reduce its side effects. the leflunomide (Arava®) can be used in people who have a contraindication or side effects to metothrexate37; more rarely, it can be used in combination with methotrexate.
The other basic treatments used arehydroxychloroquine(Plaquenil®) and sulfasalazine (eg, Salazopyrine®), administered alone or preferably in combination with methotrexate.
THEazathioprine (Imuran®, Imurel® is used in certain severe polyarthritis. Each of these medicines has specific side effects.
Biotherapies or biological response modifiers
In recent years, a new class of drugs has appeared on the market. They are known as biological response modifiers, or biotherapies. Unlike other anti-rheumatic drugs, which fight the action of the immune system in nonspecific ways, these new therapies are designed to specifically target substances believed to be directly responsible for joint inflammation and destruction. Several types of biotherapies are available, among which anti-TNF agents are the most used. There are now 5 anti-TNF agents: infliximab (Remicade®), etanercept (Enbrel®) and adalimumab (Humira®), certolizumab (Cimzia®) and golimumab (Simponi®). Biotherapies that counter the effect of interleukin-1 (anakinra, Kineret®) or interleukin-6 (tocilizumab, Roactemra®), 2 substances that contribute to inflammation along with TNF are also approved in Canada. , as well as 2 other biotherapies with different mechanisms of action, rituximab (Rituxan®) and abatacept (Orencia®). These drugs are all administered by injection, some intravenously and others subcutaneously. In addition to their mechanisms of action, these drugs differ in their frequency of administration and some specific side effects.
These drugs have a very high cost and potential forserious side effects. From side effects possible of these drugs, we note in particular a reduction of the immune defenses against certain infections.
But they are also tremendously effective and have revolutionized the course of rheumatoid arthritis, removing pain, inflammation and deformities in many patients.
surgery
When joint damage makes it difficult to function well on a daily basis, surgical interventions can be performed. They restore the function of the joint, reduce pain and restore a normal appearance to a deformed joint.
- Synovectomy. It consists of completely or partially removing the synovial membrane affected by arthritis. This procedure can be performed by surgery or by injecting a chemical or radioactive product into the joint (synoviorthesis). In the latter case, the excess synovial membrane is destroyed by the injected product. These measures give good results, but relapses are possible in the more or less long term.
- Joint replacement. It is possible to replace the affected joint with an artificial joint, the prosthesis. This intervention restores mobility while reducing pain. It can also make it possible to correct a deformation. This type of surgery is sometimes suggested before the damage to the bones and joints becomes too severe.
Physical exercise
Although the rheumatoid arthritis be a painful disease, it should not preventphysical exercise, on the contrary. Exercise helps maintain maximum joint strength and flexibility while improving overall health and quality of life. The regular practice of physical activities and muscle strengthening are part of the international recommendations, provided they are adapted to the physical health of each individual. In fact, it is important not to put too much strain on severely damaged joints and not to force in the event of painful outbreaks. The exercices aerobic are recommended, as is walking, swimming or cycling. Ask your doctor or an exercise specialist for advice.
Physiotherapy and rehabilitation
Physiotherapy and rehabilitation are useful supplements to drug treatment as soon as the disease becomes disabling (and even before, in prevention). The physiotherapist helps to find physical exercises that allow to preserve as much as possible the flexibility of the joints and to avoid deformations. If the disease causes significant disability, rehabilitation sessions can help regain autonomy and live better with this handicap. The occupational therapist can offer concrete solutions to people with rheumatoid arthritis so that they can go about their daily tasks without too much difficulty. For example, several tools or devices can prevent wrist pain, and certain postures reduce pain and fatigue.
The intervention of a physiotherapist, and in some cases an occupational therapist, helps to maintain physical capacities, both in personal and professional life.
Food
Adopting good eating habits is essential in order to maintain good health and avoid being overweight, which can make symptoms worse. The intake of antioxidants, which are found in good quantities in fruits and vegetables, is essential.
here are a few tips54 concerning fruits and vegetables:
– Eat at least one dark green vegetable (broccoli, romaine lettuce and spinach) every day.
– Eat at least one orange vegetable (carrots, sweet potatoes and winter squash) every day.
– Choose vegetables and fruits prepared without fat, sugar or salt or with few of these ingredients.
– Instead of frying your vegetables, eat them steamed or baked or sautéed
It is observed that a diet rich in fat, protein and cold meats tends to cause more pain35. However, according to the Arthritis Society of Canada, no food or diet can completely suppress arthritis symptoms.
dietary recommendations offered by nutritionist Hélène Baribeau in our Made-to-measure diet: Rheumatoid arthritis sheet.
Omega-3 fatty acids would present an interesting effect49 in combination with conventional medication, to achieve faster remission and decrease the rate of treatment failure. They can be taken in the diet (linseed oil, rapeseed, walnut, fish), or as a supplement (3 grams per day)
A glass of alcohol per day seems to tend to improve rheumatoid arthritis symptoms. But two drinks a day would tend to make it worse. The ideal is undoubtedly to stick to recommendations such as: 1 glass of alcohol per day maximum with at least one day per week without alcohol.
Vegetarian diets have been shown to be of long-term benefit in some people with rheumatoid arthritis54. This effect may be related to the decrease in saturated fat consumption and the increase in the amount of fruits and vegetables ingested, as well as whole grains, factors that may improve inflammation. Overall, any anti-inflammatory diet could prove beneficial.
The elimination of certain foods is offered by many different diets to help improve symptoms of rheumatoid arthritis. Their interest has not been scientifically demonstrated. However, on an individual basis, they could sometimes be of interest, particularly in the event that an allergic reaction to a food occurs, which may then, perhaps, exacerbate the autoimmunity involved in the disease.
For people wishing to test these diets, it is recommended not to cut out multiple foods at the same time, but rather to talk to your doctor before doing a test stopping a food for 4 to 6 weeks in order to observe the reactions of the body. Then, after 6 weeks, talk to your doctor again to define a course of action: whether or not to remove this food, and how to compensate for its eviction if it is the chosen course. The foods concerned can be dairy products, animal fats, meat and fish, cereals containing gluten, citrus fruits, eggs. Be careful not to remove everything without medical advice and not to expose yourself to food deficiencies harmful to health.
Psychological support
Expert societies recommend taking into consideration the psychological impact of rheumatoid arthritis. The intervention of a psychotherapist can sometimes be very beneficial. The cognitive and behavioral therapies, for example, help sufferers to better manage pain and illness. The different patient associations can also provide important emotional support. See the Sites of Interest and Support Groups sections.