Contents
Islets of Langerhans
Islets of Langerhans are cells in the pancreas that play an essential role in the body. They contain beta cells that secrete insulin, a hormone that regulates blood sugar. In people with type 1 diabetes, it is precisely these cells that are destroyed. The islets of Langerhans are therefore at the heart of therapeutic research.
Anatomy
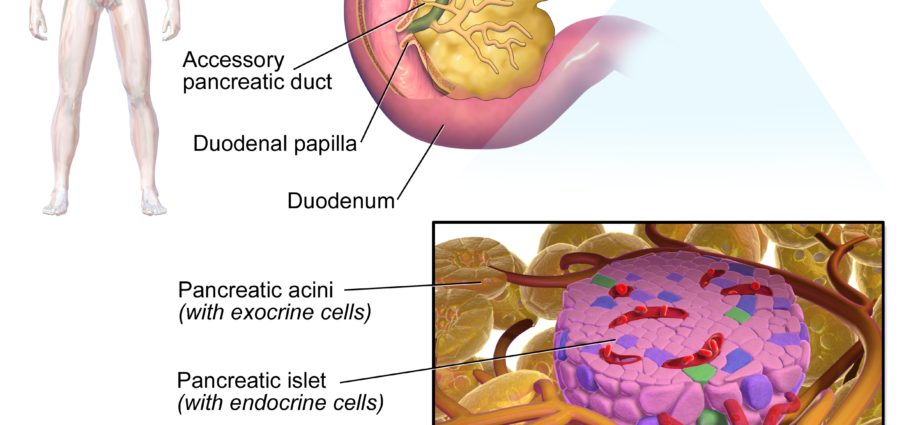
The islets of Langerhans (named after Paul Langherans, 1847-1888, German anatomo-pathologist and biologist) are cells of the pancreas, which has about 1 million. Made up of cells grouped into clusters – hence the term islets – they are disseminated in the exocrine tissue (tissue secreting substances released outside the bloodstream) of the pancreas, which in turn produces the enzymes necessary for digestion . These microscopic clusters of cells make up only 1 to 2% of the cell mass of the pancreas, but they play an essential role in the body.
physiology
Islets of Langerhans are endocrine cells. They produce different hormones: mainly insulin, but also glucagon, pancreatic polypeptide, somatostatin.
It is the beta cells or β cells of the islets of Langerhans that produce insulin, a hormone that plays a vital role in the body. Its role is to maintain the balance of the level of glucose (glycemia) in the blood. This glucose serves as a source of energy – in short, “fuel” – for the body, and its level in the blood should not be too low or too low for the body to function properly. It is precisely the role of insulin to balance blood sugar levels by helping the body to use and / or store this glucose depending on whether it is in excess or insufficient.
A cells produce glucagon, a hormone that increases the amount of glucose in the blood when blood sugar is low. It causes the liver and other tissues in the body to release stored sugar in the blood.
Anomalies / Pathologies
Diabetes type 1
Type 1 or insulin-dependent diabetes is due to the progressive and irreversible destruction of the beta cells of the islets of Langerhans by an autoimmune process of genetic cause. This destruction leads to a total insulin deficiency, and therefore a risk of hyperglycemia when food is taken, then hypoglycemia between meals, in the event of fasting or even physical activity. During hypoglycemia, the organs are deprived of an energetic substrate. If it is not regulated, diabetes can therefore induce serious renal, cardiovascular, neurological, gastroenterological and ophthalmological pathologies.
Neuroendocrine tumor of the pancreas
It is a relatively uncommon type of pancreatic cancer. It is a so-called neuroendocrine tumor (NET) because it starts in the cells of the neuroendocrine system. We then speak of NET of the pancreas, or TNEp. It can be non-secreting or secreting (functional). In the latter case, it then causes an excessive secretion of hormones.
Treatments
Diabetes type 1
Insulin therapy compensates for the lack of insulin production. The patient will inject insulin several times a day. This treatment must be followed for life.
Pancreas transplant developed in the 90s. Often coupled with a kidney transplant, it is reserved for severely affected diabetic patients 1. Despite good results, pancreatic transplantation has not become the treatment of choice for type 1 diabetes, mainly due to the cumbersome nature of the procedure and the associated immunosuppressive treatments.
Langerhans islet grafting is one of the great hopes in the management of type 1 diabetes. It consists in transplanting only the useful cells, in this case the islets of Langerhans. Taken from the pancreas of a brain-dead donor, the islets are isolated and then injected through the portal vein into the patient’s liver. One of the difficulties lies in the technique of isolating these islets. It is indeed very difficult to extract these microscopic clusters of cells from the rest of the pancreas without damaging them. The first transplants were performed in Paris in the 80s. In 2000, the Edmonton group obtained insulin independence in 7 consecutive patients transplanted with islets. Work continues around the world. In France, a multicenter clinical trial began in 2011 in 4 large Parisian hospitals united within the “Ile-de-France group for the transplantation of islets of Langerhans” (GRIIF). The results are promising: after the transplant, half of the patients are weaned off insulin, while the other half achieve better glycemic control, reduced hypoglycemia and insulin requirements.
Along with this work on transplants, research continues to understand the growth and function of these cells, as well as the genesis and development of the disease. The infection of beta cells by a herpes virus (which could be responsible for a form of diabetes specific to populations of African origin), the mechanisms of growth and maturation of beta cells, the influence of certain genes involved in the onset of the disease are part of current research avenues. The idea is indeed to discover the factors that trigger the activation of T lymphocytes against beta cells, to find solutions to block this autoimmune reaction, to regenerate the islets of Langerhans, etc.
Neuroendocrine tumor of the pancreas
The management depends on the nature of the tumor and is based on different axes:
- surgery
- chemotherapy
- antisecretory treatments to decrease hormonal secretions from the tumor
Diagnostic
Diabetes type 1
Type 1 diabetes is a disease of autoimmune origin: T lymphocytes begin to recognize molecules present in beta cells as infectious agents to be eliminated. However, symptoms appear several months or even years after this process begins. These are episodes of hypoglycaemia and / or significant weight loss despite a good appetite, frequent and abundant urination, abnormal thirst, severe fatigue. The diagnosis is made through the detection of autoantibodies in the blood.
Neuroendocrine tumor
Neuroendocrine tumors are difficult to diagnose due to the diversity of their symptoms.
If it is a functional neuroendocrine tumor of the pancreas, it can cause excessive insulin production. The appearance or worsening of initially non-insulin-dependent diabetes should also be investigated in men over 40 years of age without a family history of diabetes.
An anatomopathological examination of the tumor makes it possible to specify its nature (differentiated or undifferentiated tumor) and its grade. A complete assessment of the extension of the disease in search of metastases is also done.