Contents
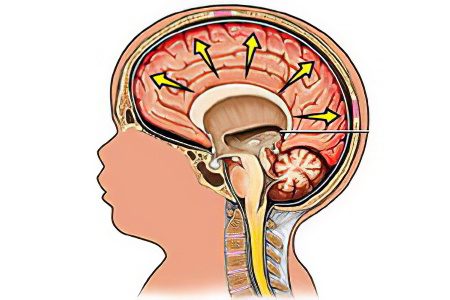
Hydrocephalus, or dropsy of the brain, is a pathology of the central nervous system, provoked by a violation of the formation, circulation and absorption of cerebrospinal fluid. Another name for the pathology, dropsy of the brain, is not entirely accurate, since the cerebrospinal fluid, or cerebrospinal fluid, is not water, but the products of the choroid plexuses of the ventricles. It washes the brain and spinal cord, filling not only the ventricles, but also the subarachnoid and subdural spaces.
The cerebrospinal fluid transports hormones, biologically active substances and nutrients, protects the brain from possible physical influences, and removes metabolic waste. In addition, cerebrospinal fluid stabilizes intracranial pressure, provides nutrition to the brain and its homeostasis, and protection from pathogenic microorganisms. Therefore, any pathological changes in the cerebrospinal fluid negatively affect the functioning of the central nervous system.
Classification
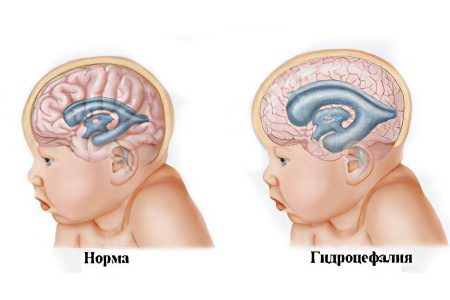
Internal hydrocephalus is the accumulation of cerebrospinal fluid in the ventricles of the brain, excluding the subarachnoid space. Almost 90% of patients with a similar diagnosis are children born with this pathology, who received it during fetal development. In adults, internal hydrocephalus occurs several times less frequently.
Forms of internal hydrocephalus, depending on the cause of its occurrence:
Communicating, or open – develops as a result of malabsorption of CSF or its hypersecretion;
Occlusive, or closed – develops if the cerebrospinal fluid circulation paths are blocked by adhesions, tumors, changes that have occurred as a result of the inflammatory process.
The prognosis of the course of the closed form is often unfavorable, it depends on how operable such changes are.
Forms of the disease depending on the time of its course and the severity of symptoms:
Acute – fixed in the first few days of the course of hydrocephalus, rapidly progressing;
Subacute – severe symptoms are diagnosed during the first month of the disease;
Chronic – the disease passes into this phase for 6-10 months or more.
The moderate form of the disease practically does not manifest itself as significant symptoms, and is accidentally detected when examining brain structures for other reasons. Sometimes it is detected when cerebrovascular accidents and functional changes in the brain parenchyma are already irreversible.
Types of the disease depending on the dynamics of its development:
Progressive hydrocephalus – symptoms are actively increasing, the volume of cerebrospinal fluid is rapidly increasing;
Stabilizing, or passive hydrocephalus – the progression of the disease does not occur;
Regressive hydrocephalus – spontaneous healing occurs.
When diagnosing, internal hydrocephalus is determined in one of three stages:
Compensated stage – no treatment is prescribed, recovery occurs spontaneously.
Subcompensated stage – some of the symptoms do not disappear without drug treatment.
Decompensated stage – the negative impact of pathology on the functioning of the brain is so significant that surgical treatment is required.
Depending on the severity of intracranial pressure, there are:
Hypertensive form – with increased ICP;
Normotensive form – the level of pressure is normal;
Hypotensive form – with reduced ICP.
Causes of internal hydrocephalus
It is necessary to distinguish between congenital and acquired factors that contribute to the development of the disease in newborns, in older children, and in adults.
Causes of the congenital form of the disease:
Infections suffered by a pregnant woman in the early stages of fetal development (rubella, mumps, herpes, cytomegalovirus, syphilis, influenza, respiratory infection);
Genetically determined pathologies;
Violations of the anatomy of the fetal brain due to intoxication (smoking during pregnancy, drinking alcohol);
Metabolic disorders due to hepatic or renal insufficiency of the fetus;
Oxygen starvation of the fetus, pathology of its circulatory system;
Fetal brain injury.
Causes of the disease that arose in early childhood:
Birth injury;
Hypoxia in childbirth;
Neuroinfections (meningitis, encephalitis);
Hemorrhages in the ventricles of the brain;
Vascular disorders;
brain tumors of any etiology;
Genetic diseases, one of the symptoms of which is external hydrocephalus.
Causes of the disease in adults:
Traumatic brain injury, complicated by cerebral hemorrhage;
Consequence of a stroke, aortic aneurysm;
Malignant brain tumor;
Complications of neuroinfections;
Diabetes;
Alcoholism;
Addiction;
Violation of cerebral circulation as a result of a stroke.
Symptoms of internal hydrocephalus
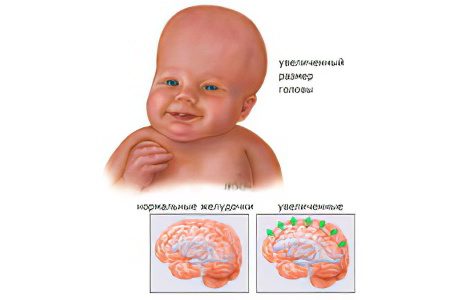
The manifestations of the disease in children under one year old are due to the fact that the bones of the skull are still mobile, and the sutures between them have not completely ossified, the fontanelles have not been tightened.
Symptoms of internal hydrocephalus in infants:
A pronounced venous network under the thin skin of the skull;
Refusal to suck, due to painful sensations due to sucking movements and the subsequent increase in intracranial pressure;
Vomiting;
Lag in weight gain;
Excessive increase in head circumference;
Moody, restless behavior;
Graefe’s syndrome, or “setting sun” syndrome, when the sclera of the eye is visible above its iris;
Delay of psychomotor development (ability to crawl, sit, walk);
Drowsiness;
Convulsions.
Symptoms of internal hydrocephalus in children of preschool and primary school age:
Irritability;
Sleep and appetite disturbances;
Violations of cognitive functions (intelligence, memory, attention);
Headaches, more common in the morning;
Violations of large and small motor skills;
visual disturbances;
Problems in teaching at school.
Not always children suffering from internal hydrocephalus have pathologies of intellectual activity. They can have excellent abilities for playing music, counting, good mechanical memory.
Symptoms of the disease in adults:
Violations of memory, intelligence, thinking;
Unsteadiness of gait, incorrect movements due to disruption of the functioning of the vestibular apparatus;
Headache not relieved by pain medications
Visual impairment, pressure on the eye sockets from the inside;
Mental disorders (aggression, emotional instability, apathy, neurasthenia);
Decreased muscle tone, development of contractures in the joints).
Some of the symptoms appear in elderly patients, and are taken by them for symptoms of aging, but not diseases.
Diagnosing

An experienced pediatric neuropathologist can easily determine the disease in a child by visual signs – the appearance of the pupils, an enlarged skull.
Methods for diagnosing a disease in adults:
Magnetic resonance imaging is an informative study that allows you to accurately determine the form and features of the pathology;
Angiography – X-ray of blood vessels using a contrast agent, which allows to assess violations of the circulatory system of the brain;
The study of cerebrospinal fluid, taken as a result of puncture.
The data obtained as a result of the study underlie the treatment strategy prescribed by the doctor.
Methods of treatment of internal hydrocephalus

Therapy of the disease in most cases is carried out in a complex, depending on the stage of the disease. At the beginning of the disease, drugs are prescribed to reduce intracranial pressure and reduce the volume of cerebrospinal fluid in the ventricles of the brain. Most often these are diuretics, vasodilators, vitamin complexes. For the treatment of children, play therapy, physiotherapy exercises, and music are used.
If drug therapy does not reduce the intensity of the symptoms of internal hydrocephalus, surgical treatment is used. The main method of alleviating the patient’s condition is shunting – the installation of a shunt connecting the ventricular cavity with the body cavity, into which CSF can be removed.
Ways of excretion of cerebrospinal fluid:
into the abdominal cavity;
into the atrium;
into the ureter;
In a container located outside the patient’s body.
There is a more modern sparing method of treatment – this is ventriculoperitoneal neuroendoscopic shunting. With the help of miniature surgical instruments and an endoscope camera, a gentle operation is performed to create artificial routes for the removal of cerebrospinal fluid from the ventricles. Most often, CSF is excreted into the occipital cistern of the brain.
To prevent the disease, pathologies of fetal development should be detected in a timely manner, and infections should be avoided. Young children should be protected from traumatic brain injuries and neuroinfections. Adults should take the same precautions.









