Contents
Hyperprolactinemia: what links between prolactin and pregnancy?
A hormone essential for the good progress of breastfeeding, prolactin is secreted in high doses at the end of pregnancy and in the weeks following childbirth. Outside of this perinatal period, however, high prolactin levels can affect fertility. Explanations.
Prolactin, what is it?
Prolactin is a hypohyseal hormone. Its role: to prepare the breast to produce breast milk and promote the growth of the mammary glands from puberty in women. In both sexes, it has feedback on the hypothalamic cells that secrete GnRH (hormone that stimulates the production of sex hormones.)
Secreted during and outside pregnancy, throughout the day, it varies under the effect of several factors:
- a diet rich in proteins or sugars,
- sleep, – stress (physical or psychological),
- possible anesthesia,
- taking certain medications.
The production of prolactin also changes during the menstrual cycle. It thus reaches its highest level at mid-cycle, in parallel with the peaks of LH hormones and estradiol. It also remains elevated during the luteal phase.
Prolactin during and after pregnancy
Prolactin and pregnancy, then prolactin and breastfeeding are intimately linked. If the normal level of prolactin is less than 25 ng / ml, it can rise to 150-200 ng / ml at the end of pregnancy and peak after birth. Indeed, after childbirth and especially after delivery, the levels of progesterone but especially estrogen drop sharply, thus releasing prolactin. The flow of milk can take place.
Subsequently, the more the child teats, the more prolactin and oxytocin (essential hormone of breastfeeding) are secreted, the more breast milk is produced regularly. About 15 days after birth, the level of prolactin begins to drop and returns to its normal level about 6 weeks after birth.
When prolactin interferes with fertility
Apart from pregnancy, a high prolactin level can be the indicator of a pathology having a significant impact on fertility: hyperprolactinemia. At the origin of this phenomenon: excess prolactin alters the secretion of GnRH, the hormone releasing pituitary gonatrophins, itself responsible for the production of hormones LH (luteinizing hormone) and FSH (follicle stimulating hormone ). However, these same hormones play a key role in ovulation. This is how we easily recognize the main symptom of hyperprolactinemia in women: amenorrhea.
His other signs:
- oligomenorrhea (infrequent and irregular cycles),
- a short luteal phase,
- galactorrhea (rush of milk),
- infertility.
Hyperprolactinemia: a male pathology too
More surprisingly, an elevated prolactin level can also be diagnosed in humans. More complex to identify, its symptoms are associated with the size of the existing tumor (headache, etc.). Hyperprolactemia can also be accompanied by other signs such as:
- loss of desire,
- erectile dysfunction,
- gynecomastia (development of the mammary glands),
- galactorrhée,
- infertility.
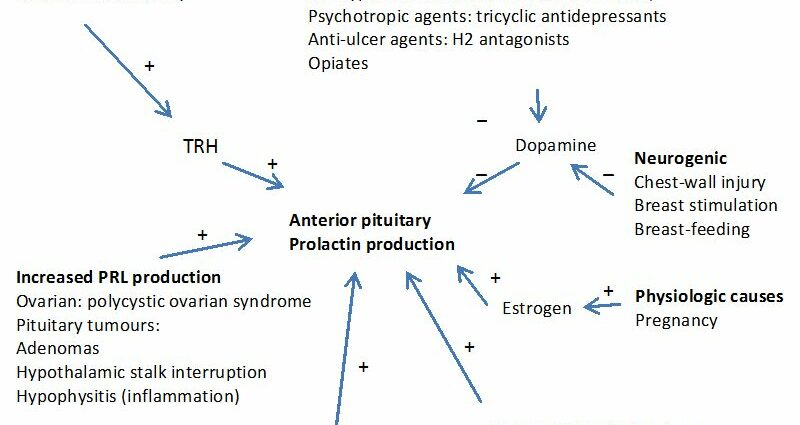
Causes of hyperprolactinemia
How to explain hyperprolactinemia? In the majority of cases, iatrogenic causes, i.e. effects of prior medical treatment, are responsible for the abnormal rise in prolactin. The main drugs involved are:
- neuroleptics,
- tricyclic antidepressants,
- metoclopramide and domperidone,
- high-dose estrogen (the contraceptive pill does not cause hyperprolactinemia),
- some antihistamines
- certain antihypertensives,
- opioids.
Second most common cause in hyperprolactinemia: microadenomas, benign tumors whose size does not exceed 10 mm, formed in the pituitary gland. Rarer, macroadenomas (larger than 10 mm in size) are accompanied not only by elevated prolactin levels, but also by headaches and ophthalmologic symptoms (restricted field of vision).
Other origins of hyperprolactinemia can be sought in hypothalamic-pituitary dysfunction including a hypothalamic tumor (craniopharyngioma, glioma) or an infiltrative disease (sarcoidosis, X-hystocytosis, etc.).
Finally, certain pathologies can involve a sharp increase in the level of prolactin, such as:
- micropolycystic ovary syndrome (PCOS),
- hypothyroidism,
- chronic renal failure,
- Cushing’s syndrome,
- other tumors or lesions of the hypothalamus.