Contents
Hemolytic anemia
Medical description
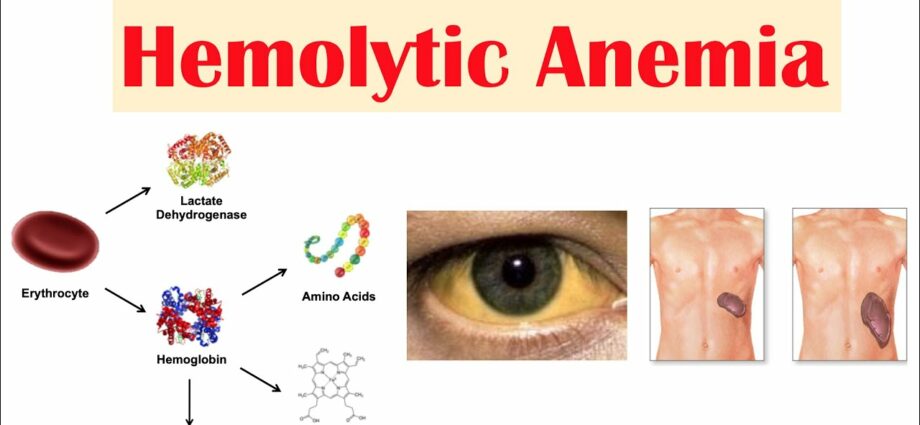
Anemia, by definition, involves a decrease in red blood cells, or hemoglobin levels. The term “hemolytic anemia” encompasses different types of anemia where red blood cells are destroyed prematurely in the blood. The term “hemolysis” means destruction of red blood cells (hemo = blood; lysis = destruction).
The bone marrow has a certain reserve capacity. That is, it can increase its production of red blood cells to a certain level to compensate for their increased destruction. Normally, red blood cells circulate in the blood vessels for about 120 days. At the end of their life, they are destroyed by the spleen and the liver (see also the Anemia sheet – overview). The accelerated destruction of red blood cells is an important stimulus in the production of new red blood cells, which is mediated by a hormone produced by the kidneys, erythropoietin (EPO). In some cases, the bone marrow is able to produce as many red blood cells as the amount that is abnormally destroyed, so the hemoglobin level does not drop. We are talking about compensated hemolysis, without anemia. This is important because there are certain factors that can cause the situation to decompose into factors that will interfere with EPO production such as pregnancy, kidney failure, folic acid deficiency, or acute infection.
Causes
Hemolytic anemia is generally classified according to whether it is caused by a red blood cell which is itself abnormal (intracorpuscular), or a factor which is external to the red blood cell (extracorpuscular). A distinction is also made between hereditary and acquired hemolytic anemia.
Hereditary and intracorpuscular causes
- Hemoglobinopathies (eg sickle cell anemia, etc.)
- Enzymopathies (eg G6-PD deficiency)
- Membrane and cytoskeletal abnormalities (eg congenital spherocytosis)
Hereditary and extracorpuscular cause
- Familial hemolytic-uremic syndrome (atypical)
Acquired and intracorpuscular cause
- Paroxysmal nocturnal hemoglobinuria
Acquired and extracorpuscular cause
- Mechanical destruction (microangiopathy)
- Toxic agents
- pharmaceuticals
- Infections
- Immunological
Let’s discuss a few examples then, since it is impossible to describe them all in the context of this document.
Immunological hemolytic anemias:
Autoimmune reactions. In this case, the body, for various reasons, produces antibodies against its own red blood cells: these are called autoantibodies. There are two types: those with hot autoantibodies and those with cold autoantibodies, depending on whether the optimum temperature for antibody activity is 37 ° C or 4 ° C. This distinction is important because treatment varies from form to form.
– Hot autoantibodies: mainly affect adults and cause chronic and sometimes severe hemolytic anemia. They represent 80% of autoimmune hemolytic anemias. In half of the cases, they can be triggered by certain drugs (alpha-methyldopa, L-dopa) or certain diseases (ovarian tumor, lymphoproliferative syndrome, etc.). This is referred to as “secondary” autoimmune hemolytic anemias, since they appear as a result of another disease.
– Cold auto-antibodies: are associated with acute episodes of destruction of red blood cells caused by cold. In 30% of cases, we are dealing with a secondary autoimmune reaction which can be explained by a viral infection or a mycoplasma, an intermediate microorganism between viruses and bacteria.
Immunoallergic reactions. In case of immunoallergic (non-autoimmune) drug hemolysis, the antibodies do not attack red blood cells, but certain drugs: penicillin, cefalotin, cephalosporins, rifampicin, phenacetin, quinine, etc.
Congenital hemolytic anemias:
There are three essential components in red blood cells. There is hemoglobin, the membrane-cytoskeleton complex, and the enzymatic “machinery” to make it all work. Genetic abnormalities in any of these three factors can cause hemolytic anemia.
Hereditary abnormalities of the membrane of red blood cells. The main one is congenital spherocytosis, so named because of the spherical shape which then characterizes the red blood cells and which makes them particularly fragile. It is relatively frequent: 1 case in 5000. Several genetic abnormalities are involved, the classic form is autosomal dominate, but recessive forms also exist. It can cause certain complications: gallstones, ulcers on the legs.
Enzymopathies. There are several forms of enzyme deficiency that can cause hemolytic anemia. They are generally hereditary. The most common is a deficiency in an enzyme called “glucose-6-phosphate dehydrogenase”, which causes premature destruction of red blood cells and, subsequently, hemolytic anemia.
The genetic defect that is involved is linked to the X chromosome, therefore, only men can be affected. Women can carry the genetic defect and pass it on to their children. In people with this enzyme deficiency, hemolytic anemia most commonly occurs following exposure to oxidizing agents.
People with G6PD deficiency can develop acute hemolysis when exposed to certain agents such as:
– consumption of the variety of beans called small-grain bean (addictive faba) or exposure to pollen from that plant (this variety of beans is used for livestock feed). This contact results in acute hemolytic anemia also called favism.
– the use of certain drugs: antimalarials, methyldopa (lowers blood pressure), sulfonamides (antibacterials), aspirin, non-steroidal anti-inflammatory drugs, quinidine, quinine, etc.
– exposure to certain chemicals such as mothballs.
– certain infections.
This disease is frequently diagnosed in people from the Mediterranean Basin (especially the Greek Islands) as well as black people in Africa and the United States (where its prevalence is 10% to 14%). In some parts of the world, 20% or more of the population has it.
An example of convergent evolution One might wonder why a genetic defect is so common. One might expect that the principle of Darwinian selection would mean that over time there are fewer and fewer people affected. The reason is that this anomaly confers a certain advantage for survival! In fact, those affected are relatively protected against malaria. Also, the genes involved are different in different parts of the world, this heterogeneity testifies that these genes were selected by the selection pressure caused by malaria. This is a case of convergent evolution. |
Hemoglobinopathies. Term used to describe genetic diseases where the production of hemoglobin inside red blood cells is affected. Sickle cell anemia (sickle cell anemia) and thalassemia are the two main categories of hemoglobinopathies.
Sickle cell anemia (sickle cell anemia)4,5. This relatively serious disease is linked to the presence of an abnormal hemoglobin called hemoglobin S. This distorts the red blood cells and gives them the shape of a crescent or a scythe (sickle cells), in addition to causing them to die. prematurely. See the sheet Sickle cell anemia.
Thalassemia. Very widespread in certain countries of the world, this serious disease is linked to a genetic abnormality that affects the production of hemoglobin, this blood pigment in red blood cells that allows the transport of oxygen to organs. Affected red blood cells are fragile and quickly broken down. The term “thalassemia” comes from the Greek word “thalassa”, which means “sea”, as it was first observed in people from the Mediterranean basin. The genetic defect can affect two places in the synthesis of hemoglobin: the alpha chain or the beta chain. Depending on the type of chain affected, there are two forms of thalassemia: alpha-thalassemia and beta-thalassemia.
Other causes
Mechanical causes. Red blood cells can be damaged during certain treatments related to mechanical devices:
– prostheses (artificial valves for the heart, etc.);
– extracorporeal blood purification (hemodialysis);
– machine to oxygenate the blood (used in heart-lung surgery), etc.
Rarely, a marathon runner may experience mechanical hemolysis as the capillaries in the feet are repeatedly crushed. This situation has also been described after certain very prolonged ritual dances, on bare feet.
Exposure to toxic elements.
– Industrial or domestic toxic products: aniline, arsenic hydrogen, nitrobenzene, naphthalene, paradichlorobenzene, etc.
– Toxic animal: spider bite, wasp sting, snake venom.
– Plant poisonous: certain fungi.
Infections.Severe gastroenteritis caused by And coli, infections caused by pneumococcus or staphylococcus, hepatitis, typhoid fever, malaria, etc. Malaria (or malaria) is the most important cause in this category. Malaria is caused by a parasite that grows inside the red blood cells.
Hyperfunction of the spleen. It is normal for red blood cells to be destroyed in the spleen after their 120-day journey, but if this organ functions excessively, the destruction is too rapid and hemolytic anemia ensues.
Hemoglobinuria paroxysmal nocturnal. This chronic disease is associated with the presence of hemoglobin in the urine due to excessive destruction of red blood cells. Nighttime seizures are caused by any form of stress, immune system stimulation or certain medications. Sometimes the disease causes lower back pain and discomfort.
Possible complications: thrombosis, bone marrow hypoplasia, secondary infections.
Symptoms of the disease
- Those linked to a low level of red blood cells: pale complexion, fatigue, weakness, dizziness, rapid heartbeat, etc.
- Jaundice.
- Dark urine.
- Enlargement of the spleen.
- Those that are specific to each form of hemolytic anemia. See “Medical Description”.
People at risk
For congenital forms of hemolytic anemia:
- Those with a family history.
- People from the Mediterranean basin, Africa, South and Southeast Asia and the West Indies.
Risk factors
- In people with a deficiency of the enzyme glucose-6-phosphate dehydrogenase: exposure to oxidizing agents (certain drugs, field bean, etc.).
- For other forms of hemolytic anemia:
– Certain diseases: hepatitis, streptococcal infection or E. coli, autoimmune disorders (such as lupus), ovarian tumor.
– Certain drugs (antimalarials, penicillin, rifampicin, sulfonamides, etc.) or toxic agents (aniline, arsenic hydrogen, etc.).
– Certain mechanical devices used in medicine: artificial valves, devices for purifying or oxygenating the blood.
— Stress.
Prevention
- At present, it is impossible to prevent hereditary forms except by consulting a genetic counselor before conceiving a child. The specialist will be able to determine the risks of giving birth to a child with hemolytic anemia when either (or both) of the potential parents has a family history (see also Sickle Cell Anemia for more details on the genetic risks with regard to this form of hemolytic anemia).
- If a specific substance is responsible for the disease, it should be avoided to prevent recurrences.
- For many forms of hemolytic anemia, it is also important to guard against certain infections.
Medical treatments
They vary depending on the type of hemolytic anemia.
- Treatment is first and foremost based on general support to the body and the underlying cause when possible
- A supplement of folic acid is generally indicated for patients with chronic hemolytic anemia.
- Vaccination against common infections is important for those patients who have impaired immune defenses, especially in people with splenectomies (removal of the spleen6)
- Blood transfusions are sometimes indicated
- Splenectomy is sometimes suggested7, especially in people with hereditary spherocytosis, thalassemias which often require transfusions but also sometimes in other forms of chronic hemolytic anemia. Indeed, it is largely in the spleen that red blood cells are destroyed.
- Cortisone is sometimes prescribed for hot antibody autoimmune anemia and to consider for cold antibody anemia. It is sometimes used in cases of paroxysmal nocturnal hemoglobinuria and in particular for thrombotic thrombocytopenic purpura. Stronger immunosuppressive agents, such as rituximab8, intravenous immunoglobulins, azathioprine, cyclophosphamide, and cyclosporine may be considered in immunologic hemolytic anemias. Plasmapheresis is sometimes used, in particular in the case of this thrombotic thrombocytopenic purpura.
The doctor’s opinion
As part of its quality approach, Passeportsanté.net invites you to discover the opinion of a health professional. Dr Dominic Larose, emergency physician, gives you his opinion on the hemolytic anemia :
Hemolytic anemia is a relatively complex subject which necessarily requires specialized investigation. You will therefore need to work together with a competent medical team who will be able to guide you in making the best choices. Dr Dominic Larose, M.D. CMFC(MU) FACEP |
Medical review: December 2014 |
Complementary approaches
The only unconventional treatments identified concern sickle cell anemia. See this sheet for more details.