Contents
- What is Basedow’s disease
- Photos before and after Graves’ disease
- Causes of Basedow’s disease in adults
- Who is more likely to get Graves’ disease?
- Symptoms of Basedow’s disease in adults
- Treatment of Basedow’s disease in adults
- Prevention of Basedow’s disease in adults at home
- Popular questions and answers
The thyroid gland is a relatively small organ of the endocrine system located under the skin on the front of the neck. Its main task is the release of thyroid hormones that regulate the basic metabolism (the release of energy for the vital activity of cells and tissues). If, for various reasons, the gland begins to work more actively than usual, this can lead to Graves’ disease in adults.
This name has traditionally remained since the days of Soviet medicine and is now considered obsolete. In international literature and clinical guidelines, the name hyperthyroidism or Graves Disease is used. Other names that are used in various countries include these synonyms:
- exophthalmic goiter;
- Graves’ hyperthyroidism;
- Parry’s disease;
- toxic diffuse goiter.
In addition, there is also an internal division of Graves’ disease, depending on the predominance of certain symptoms:
- dermopathy (when the skin is especially affected);
- osteopathy (skeletal problems);
- ophthalmopathy (mainly eye symptoms).
What is Basedow’s disease
Graves’ disease or Graves’ thyroiditis is a disease that affects the thyroid gland, as well as the skin and eyes.
The thyroid gland is an organ that is part of the endocrine system, a network of endocrine glands and tissues that secrete hormones that regulate chemical processes (metabolism).
Hormones affect the vital functions of the body, and also regulate heart rate, body temperature and blood pressure. Hormones are released directly into the bloodstream, from where they travel to various areas of the body.
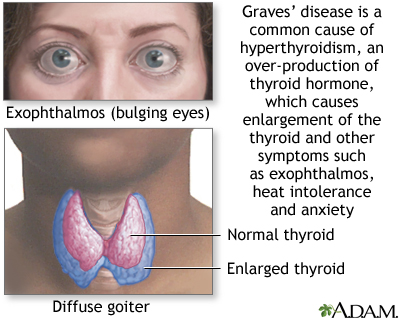
Graves’ disease is characterized by abnormal enlargement of the thyroid gland (called a goiter) and increased secretion of thyroid hormone (hyperthyroidism). Thyroid hormones are involved in many different body systems and, as a result, the specific symptoms and signs of Graves’ disease can vary widely among people of different sex and age. Common symptoms include unintentional weight loss, abnormal heat intolerance with profuse sweating, muscle weakness, fatigue, and eyeball protrusion. Graves’ disease is inherently an autoimmune disease.
Photos before and after Graves’ disease
Causes of Basedow’s disease in adults
Graves’ disease is considered an autoimmune disease, but other factors, including genetic, environmental, or environmental factors, may contribute to its development. Autoimmune disorders occur when the body’s immune system mistakenly attacks healthy tissues.
The immune system normally produces specialized proteins called antibodies. These antibodies react to foreign materials (eg bacteria, viruses, toxins) in the body, causing them to be destroyed. Antibodies can directly kill microorganisms or coat them so that they are more easily broken down by white blood cells. Specific antibodies are created in response to certain materials or substances that stimulate the production of antibodies. They are called antigens.
In Graves disease, the immune system produces an abnormal antibody called thyroid-stimulating immunoglobulin. This antibody mimics the function of normal thyroid-stimulating hormone (which is secreted by the pituitary gland). This hormone mimic attaches to the surface of thyroid cells and causes the cells to produce thyroid hormones, resulting in an excess of them in the blood. There is hyperactivity of the thyroid gland, its enhanced, excessive work. In Graves’ ophthalmopathy, these antibodies may also affect the cells surrounding the eyeball.
Affected people may have specific defective genes or a genetic predisposition to Graves’ disease. A person who is genetically predisposed to a disease carries the gene (or genes) for that disease, but the pathology may not manifest itself if the gene is not triggered or “activated” under certain circumstances, for example, due to rapidly changing environmental factors (so-called multifactorial heredity).
Various genes have been identified that are associated with Graves’ disease, including those that:
- weaken or modify the response of the immune system (immunomodulators),
- that are directly related to thyroid function, such as thyroglobulin (Tg) or thyroid stimulating hormone receptor (TSHR) genes.
Gene Tg produces thyroglobulin, a protein that is found only in thyroid tissue and plays a role in the production of its hormones.
Gene TSHR produces a protein that is a receptor and binds to thyroid stimulating hormone. The exact basis of the interaction of genetic and environmental factors that cause Graves’ disease is not fully understood.
Additional genetic factors, known as modifier genes, may play a role in the development or expression of the disease. Environmental factors that can trigger the development of hyperthyroidism include extreme emotional or physical stress, infection, or pregnancy. People who smoke are at greater risk of developing Graves’ disease and ophthalmopathy. Individuals who have other pathologies caused by a malfunction of the immune system, such as type 1 diabetes or rheumatoid arthritis, are at greater risk of developing Graves’ disease.
Who is more likely to get Graves’ disease?
Graves’ disease affects women more often than men, at a ratio of 10:1. The disease usually develops in middle age with a maximum incidence between the ages of 40 and 60, but can also affect children, adolescents, and the elderly. Graves’ disease occurs in almost every part of the world. It is estimated that 2-3% of the population suffers from it. By the way, Graves’ disease is the most common cause of hyperthyroidism.
Other health problems and family history are also important. People with Graves’ disease often have a history of other family members with thyroid problems or autoimmune diseases. Some relatives may have had hyperthyroidism or an underactive thyroid, others may have other autoimmune diseases, including premature graying of the hair (beginning in their 20s). By analogy, a patient may have associated immune problems in the family, including juvenile diabetes, pernicious anemia (due to vitamin B12 deficiency), or painless white patches on the skin (vitiligo).
It is important to rule out other causes of hyperthyroidism. They include toxic nodular or multinodular goiter, which is characterized by one or more nodules or bumps in the thyroid gland that gradually grow and increase their activity so that the total output of thyroid hormone into the blood exceeds the norm.
Also, people may temporarily develop symptoms of hyperthyroidism if they have a condition called thyroiditis. This condition is caused by a problem with the immune system or a viral infection that causes the gland to leak stored thyroid hormone. Types of thyroiditis include subacute, silent, infectious, radiation therapy-induced, and postpartum thyroiditis.
Rarely, certain forms of thyroid cancer and certain tumors, such as TSH-producing pituitary adenomas, can cause symptoms similar to those seen in Graves’ disease. Rarely, symptoms of hyperthyroidism can also be caused by taking too much thyroid hormone in pill form.
Symptoms of Basedow’s disease in adults
The symptoms associated with Basedow’s disease usually appear gradually, sometimes even imperceptibly for the person himself (they may be the first to notice relatives). They take weeks or months to develop. Symptoms may include behavioral changes such as extreme nervousness, irritability, anxiety, restlessness, and difficulty sleeping (insomnia). Additional symptoms include unintentional weight loss (without following strict diets and nutritional changes), muscle weakness, abnormal heat intolerance, increased sweating, rapid, irregular heartbeat (tachycardia), and fatigue.
Graves’ disease is often associated with pathologies affecting the eyes, often referred to as ophthalmopathy. A mild form of ophthalmopathy is present in most people who have hyperthyroidism at some point in the disease, less than 10% of patients have significant eye involvement that requires active treatment. Eye symptoms may develop before, at the same time, or after the development of hyperthyroidism. Rarely, people with eye symptoms never develop hyperthyroidism. In some cases, eye damage may first appear or worsen after treatment for hyperthyroidism.
Complaints in ophthalmopathy are very variable. For some people, they may remain unchanged for many years, while for others, the condition may improve or worsen in just a couple of months. Changes can also follow the pattern: a sharp deterioration (exacerbation), and then a significant improvement (remission). In most people, the disease is mild and does not progress.
Common manifestations of eye symptoms are swelling of the tissues surrounding the eyeball, which can cause it to bulge out of the orbit, a condition called proptosis (bulging eyes). Patients may also note severe dryness of the eyes, swelling of the eyelids and their incomplete closure, eversion of the eyelids, inflammation, redness, pain and irritation of the eyes. Some people describe the feeling of sand in their eyes. Less commonly, blurred or double vision, sensitivity to light, or blurred vision may occur.
Very rarely, people with Graves’ disease develop a skin lesion known as pretibial dermopathy or myxedema. This condition is characterized by the appearance of thickened, reddish skin on the front of the legs. Usually it is limited to the shins, but sometimes it can also occur on the feet. Rarely, gel-like swelling of the tissues of the hands and swelling of the fingers and toes (acropachia) occur.
Additional symptoms associated with Graves’ disease include:
- cardiopalmus;
- slight tremor (trembling) of the hands and / or fingers;
- hair loss;
- brittle nails;
- increased reflexes (hyperreflexia);
- increased appetite and increased bowel movements.
Women with Graves’ disease may experience changes in their menstrual cycle. Men may experience erectile dysfunction (impotence).
In some cases, Graves’ disease can progress, causing congestive heart failure or abnormal thinning and weakness of the bones (osteoporosis), making them brittle and causing fractures from minor trauma or awkward movements.
Treatment of Basedow’s disease in adults
Diagnosis and treatment of Basedow’s disease is reflected in international protocols and national clinical guidelines. The examination plan is drawn up in strict accordance with the proposed diagnosis and is carried out in stages.
Diagnostics
The diagnosis of Graves’ disease is made on the basis of a detailed history of the patient and his family (finding out if close relatives have problems of a similar nature), a thorough clinical assessment, identification of characteristic signs, etc. After clinical symptoms are identified, laboratory tests and instrumental examinations are prescribed.
General tests (blood, urine, biochemistry) and specialized tests such as blood tests that measure levels of thyroid hormone (T3 and T4) and thyroid stimulating hormone (TSH levels) are shown. To confirm the diagnosis, blood tests may be performed to detect the presence of specific antibodies to thyrogloulin and thioperoxidase that cause Graves’ disease, but this is usually not necessary.
Modern treatments
Treatment for Graves’ disease usually involves one of three methods:
- antithyroid drugs (suppress the work of the thyroid gland on the synthesis of hormones);
- the use of radioactive iodine;
- surgical intervention.
The specific form of treatment recommended may depend on the age of the patient and the extent of the disease.
Clinical guidelines
All stages of treatment are carried out in accordance with the recommendations of the Clinical protocols
The least invasive treatment for Graves’ disease is the use of drugs that reduce the release of thyroid hormone (antithyroid drugs). They are particularly preferred for the treatment of pregnant women, those with mild hyperthyroidism, or patients requiring prompt treatment for hyperthyroidism. Specific drugs are selected by the doctor, based on the age of the patient, his condition and additional factors.
The definitive treatments for Graves’ disease are those that destroy the thyroid gland, resulting in hypothyroidism. Radioactive iodine therapy is the most common treatment for Graves’ disease in many countries. Iodine is a chemical element used by the thyroid gland to create (synthesise) thyroid hormones. Almost all iodine in the human body is absorbed by the tissues of the thyroid gland. Patients swallow a solution containing radioactive iodine, which will travel through the bloodstream and accumulate in the thyroid gland, where it will damage and destroy thyroid tissue. This will shrink the thyroid gland and reduce the overproduction of hormones. If thyroid hormone levels fall too low, hormone therapy may be needed to restore adequate thyroid hormone levels.
Another radical therapy is surgery to remove all or part of the thyroid gland (thyroidectomy). This method of treatment of the disease is usually reserved for people in whom other forms of treatment have not been successful or are contraindicated, or in the presence of growth of gland tissue to a significant size. After surgery, hypothyroidism often occurs – this is the desired result, which is corrected by a strictly adjusted dose of hormones from the outside.
In addition to the three treatments mentioned above, drugs can be prescribed that block the thyroid hormone that is already circulating in the blood (beta-blockers) from doing its job. Beta blockers such as propranolol, atenolol, or metoprolol may be used. When the level of thyroid hormones normalizes, therapy with beta-blockers can be stopped.
In many cases, lifelong follow-up and laboratory investigations are necessary. In some cases, lifelong hormone replacement therapy may be required.
Mild cases of ophthalmopathy can be treated with sunglasses, ointments, artificial tears. More severe cases may be treated with corticosteroids such as prednisone to reduce swelling in the tissues surrounding the eyes.
In more severe cases, orbital decompression surgery and orbital radiation therapy may also be required. During orbital decompression surgery, the surgeon removes the bone between the eye socket (orbit) and the sinuses. This allows the eye to return to its natural position in the socket. This surgery is usually reserved for people who are at risk for vision loss due to pressure on the optic nerve or for whom other treatment options have not worked.
Prevention of Basedow’s disease in adults at home
Predicting the development of the disease in advance and preventing it is difficult. But there are measures to reduce the risks of complications and progression of hyperthyroidism.
If Graves’ disease is diagnosed, make mental and physical well-being a priority.
Proper nutrition and exercise may improve some symptoms during treatment and help you feel better overall. For example, because the thyroid gland controls metabolism, hyperthyroidism may tend to become fuller and brittle after hyperthyroidism is corrected, and resistance exercise may help maintain bone density and weight.
Stress reduction may be beneficial as it may cause or exacerbate Graves’ disease. Pleasant music, a warm bath or a walk will help you relax and improve your mood.
Rejection of bad habits – do not smoke. Smoking worsens Graves’ ophthalmopathy. If the disease affects your skin (dermopathy), use over-the-counter creams or ointments containing hydrocortisone to relieve swelling and redness. In addition, compression leg wraps can help.
Popular questions and answers
Questions relating to Basedow’s disease, we discussed with general practitioner, endoscopist, head of the organizational and methodological office Lidia Golubenko.
Vision problems, known as thyroid disease or Graves’ ophthalmopathy, affect about 1 in 3 people with an overactive thyroid due to Graves’ disease. Problems may include:
● feeling of dryness and sand in the eyes;
● sharp sensitivity to light;
● lacrimation;
● blurred vision or double vision;
● redness of the eyes;
● wide-eyed.
Many cases are mild and improve with thyroid treatment, but about 1 in 20 to 30 cases are at risk for vision loss.
Treatment for an overactive thyroid often results in too low hormone levels. This is called an underactive thyroid gland (hypothyroidism). Symptoms of an underactive thyroid may include:
● sensitivity to cold;
● fatigue;
● weight gain;
● constipation;
● depression.
Decreased thyroid activity is sometimes temporary, but permanent and long-term treatment with thyroid hormones is often needed.
Women may have problems with pregnancy. If your thyroid is overactive during pregnancy and your condition is poorly controlled, it may increase your risk of:
● preeclampsia;
● miscarriage;
● premature birth (before 37 weeks of pregnancy);
● Your baby may have a low birth weight.
If you are not planning a pregnancy, it is important to use birth control because some treatments for Graves’ disease can harm the unborn baby.
● infection;
● the onset of pregnancy;
● incorrect medication;
● damage to the thyroid gland, such as a blow to the throat.
Symptoms of a thyroid crisis include:
● palpitations;
● high temperature;
● diarrhea and nausea;
● yellowing of the skin and eyes (jaundice);
● severe agitation and confusion;
● loss of consciousness and to whom.
An overactive thyroid can also increase your chances of developing:
● atrial fibrillation – lesions of the heart that cause an irregular and often abnormally high heart rate;
● bone resolution (osteoporosis) – a condition in which your bones become brittle and more likely to break;
● heart failure – the heart cannot properly pump blood around the body.