Contents
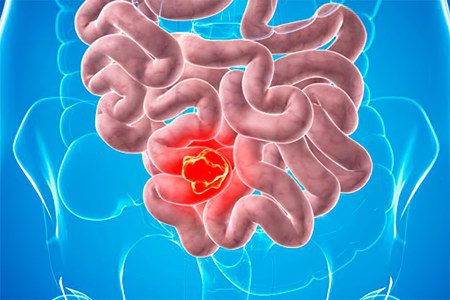
Enteritis is an inflammation of the small intestine. The disease is accompanied by dystrophic changes in the mucous membrane and can lead to serious complications. It is characterized by a violation of the processes of digestion and absorption. We learn about the causes of enteritis, symptoms, treatment, prevention, diet and other important points in order to diagnose the disease in a timely manner and fight it with effective measures.
Why is it important to treat enteritis?
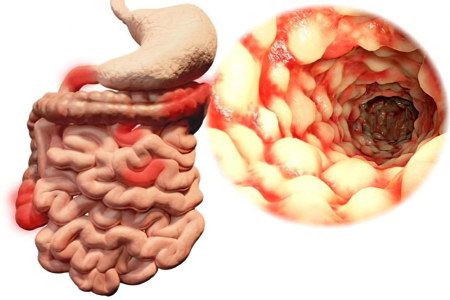
The small intestine is an important organ of the digestive system. This is a long and sinuous muscular tube that receives partially digested food from the stomach. Most of the chemical processes associated with the breakdown of food occur in the small intestine. This organ is also responsible for the absorption of the nutrients the body needs. The functionality of the small intestine is provided by finger-like microscopic protrusions – villi that extend into the lumen of the organ. The small intestine is also a habitat for beneficial microorganisms. Various bacteria contribute to the breakdown of nutrients, protect the body from pathogenic microbes. According to its anatomical structure, the small intestine consists of several parts. Infections, inflammations and diseases that occur in any segment have a negative impact on the organ and lead to disruption of the functionality of the small intestine. When entering the chronic form, enteritis requires long-term complex treatment, so you should be attentive to your health and take certain steps in a timely manner to combat the disease.
Reasons for the development of enteritis
Inflammation in the small intestine is usually the result of a viral, bacterial, or parasitic infection, such as stomach flu or food poisoning. Radiation exposure, drug exposure, or prolonged illness can also cause enteritis.
Is enteritis a dangerous disease?
Inflammation and irritation of the small intestine can lead to fever, swelling and severe pain in the abdomen. As a result, digestive disorders occur, which manifest themselves in the form of diarrhea, nausea and vomiting. Depending on the characteristics of the course of the disease, acute enteritis is isolated, which occurs suddenly and is short-lived. Less commonly, a chronic disease develops – persistent enteritis.
According to statistics, in most cases the disease does not pose a serious danger and the prognosis is good if enteritis is diagnosed in a timely manner and a treatment plan is correctly drawn up. With a disease that occurs in a mild form, you can fight at home under the supervision of a specialist. The biggest problem that can lead to complications is dehydration caused by diarrhea and vomiting.
For successful treatment, it is necessary to get more rest and replenish fluid reserves with the help of electrolyte mixtures and other special pharmaceuticals. In cases where a bacterial infection is suspected, treatment of acute enteritis may require antibiotics. With severe dehydration, the patient is hospitalized. If enteritis lasts for a long time, then it can cause more serious complications, which happens quite rarely.
The main types of enteritis and causes of development
Enteritis can be superficial, proceeding with dystrophic changes in enterocytes, or chronic, without concomitant atrophic processes. Depending on the change in the functional characteristics, enteritis can occur against the background of a violation of membrane digestion, the absorption process, or changes in intestinal motility.
Infectious enteritis
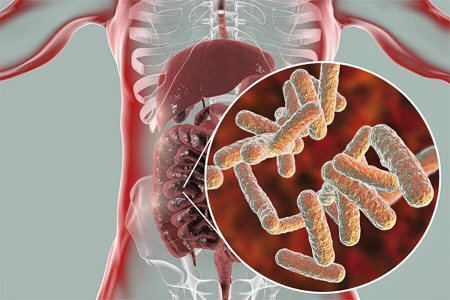
This is the most common type that develops against the background of infection with viruses, bacteria and various parasites. Pathological microorganisms enter the body through contaminated food, water, or through contact with another infected person.
Viruses that commonly cause enteritis include:
norovirus;
astrovirus;
rotavirus;
adenovirus.
Enteritis causing bacteria:
Escherichia coli;
Shigella;
salmonella.
Clostridioides difficile;
Campylobacter jejuni;
golden staphylococcus.
Parasites that cause enteritis:
lamblia;
Cyclospora;
Cryptosporidium.
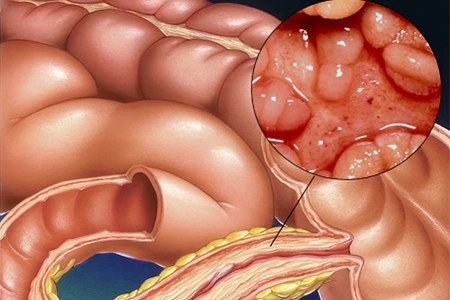
Inflammatory enteritis
Primary inflammatory enteritis is caused by certain autoimmune diseases that affect the digestive system. Inflammation develops as the immune system attacks healthy cells. This can become a chronic problem. Excessive use of certain drugs can lead to intestinal inflammation.
These include:
NSAIDs (non-steroidal anti-inflammatory drugs);
antibacterial agents.
People who abuse alcohol and drugs are also at risk.
Radiation enteritis
Radiation enteritis is caused by radiation. People with localization of the procedure in the abdominal cavity and pelvic region are especially susceptible to the disease. This is due to the fact that radiation therapy and chemotherapy are used to destroy cancer cells, but healthy tissues that are in the protective shell of the mouth, stomach and intestines are also damaged during irradiation. This contributes to the disruption of the barrier function, which leads to irritation and inflammation. In most patients, radiation enteritis occurs only a few weeks after chemotherapy treatment. In rare cases, the pathological condition persists for several months or even years. It is not yet known why this is the case, but it is well known that patients with chronic radiation enteritis may be at risk of severe damage to the small intestine.
Ischemic enteritis
Intestinal ischemic syndrome occurs when the blood supply to any part of the intestine is cut off. Small bowel ischemia, although rare, can be a serious condition that leads to enteritis and all associated typical symptoms.
The symptom is enteritis
The clinical picture of the disease is characterized by varying degrees of severity of pathological processes. The main syndrome of enteropathy is malabsorption, which may be accompanied by frequent or rare relapses.
There are two phases of the disease: exacerbation and remission, which can alternate.
Enteritis is accompanied by a violation of the functioning of the intestinal wall, resulting in a decrease in the activity of cell membranes, a change in the transport channels that promote the absorption of decay products (ions and water).
The clinic of pathology depends on the specific disorders that accompany the course of the disease, and the main manifestation of enteritis remains the syndrome of impaired absorption and diarrhea that recurs from time to time. The cause of loose stools is increased secretion of intestinal juice, high osmolarity of the contents of the small intestine, as well as a violation of the intestinal flora and the rapid passage of intestinal transit.
Typical symptoms of enteritis:
fever;
pain and cramps in the abdomen;
nausea and vomiting;
decreased appetite;
diarrhea;
blood in the stool;
white coating on the tongue;
muscle weakness;
headache;
bloating;
pallor of the skin.
All symptoms are divided into two groups: intestinal and flowing outside the walls of the intestine. Extraintestinal symptoms of the disease include malabsorption syndrome. It is expressed in a decrease in body weight of patients, and in some cases weight loss reaches 20 kilograms, lethargy, irritability, sleep disturbance.
In addition, patients experience trophic changes in the skin and its appendages: dryness, thinning, exfoliation of the upper layers of the epidermis, brittleness and hair loss, thickening of the nail plate appear. With strong manifestations of hypoproteinemia, pastosity of the skin is observed, edema appears. Patients report muscle pain, muscle weakness, decreased tendon reflexes, paresis, and increased heart rate. On the ECG, a decrease in the ST segment is noticeable, as well as flattening and two-phase T wave. Extrasystole develops, caused by a low concentration of potassium in the blood. In 2/3 of patients, there is also a decrease in the level of calcium in the bloodstream, which is accompanied by the development of muscle cramps on the part of small muscles.
Some manifestations of the disease are associated with hypovitaminosis, which develops against the background of impaired absorption of nutrients in the intestinal region. In this case, the symptoms of enteritis resemble the clinic of beriberi, characteristic of a deficiency of a number of vitamins: A, B2, K, D, B6, B12, E.
From the side of the intestine, a number of symptoms are also noted, and with the development of the pathological process only in the initial section of the jejunum, intestinal symptoms are less pronounced. When the inflammatory process affects the jejunum and ileum, there is a violation of the absorption of bile acids, which in healthy people occurs in the distal intestine. The consequence of such a violation is an excessive flow of bile into the large intestine and the development of diarrhea. The direct cause of the change in stool is an increased concentration of sodium, chlorine ions, as well as the appearance of an excess volume of water in the intestinal lumen due to the stimulating effect of bile acids on the course of these processes. An increase in the volume of feces activates the motor function of the intestine.
Violations of the functioning of the ileocecal valve cause the intestinal contents to reflux from the colon into the ileum and become contaminated with microbial flora. Prolonged intestinal reflux ileitis can cause symptoms characteristic of vitamin B12 deficiency; in severe cases, enteritis occurs with symptoms of B12 deficiency anemia. Similar manifestations of the disease are accompanied by pain in the right iliac region.
In addition, enteritis is characterized by pain in the middle of the abdomen in the navel, which appear about three hours after eating. They can be cramping, blunt or arching. When examining and determining the projection of the pain syndrome, there is pain in the jejunum, namely on the left above the navel, and the doctor can also state noise and splashing in the intestinal loops, more often in the region of the caecum.
The stool of patients is liquid, quickened, yellow in color, its frequency reaches five or more times a day. Patients are concerned about bloating, rumbling in the intestines. Juvenile diarrhea is the most severe.
Complications
Complications of acute enteritis
The most serious complication of acute enteritis is dehydration of varying severity. Adults can deal with this pathological condition associated with dehydration relatively easily. Children, the elderly and immunocompromised patients often suffer severe consequences. If you have been diagnosed with enteritis or are caring for a loved one with such a disease, then make sure that fluid reserves in the body are replenished in a timely manner.
Signs of dehydration:
headache;
muscle weakness;
fatigue;
dry mouth;
dizziness;
sunken eyes;
cardiopalmus;
low blood pressure.
dark urine;
constipation.
Complications of chronic enteritis
Although chronic enteritis resulting from radiation therapy or inflammatory bowel disease is less common, it can have serious long-term side effects that significantly impair quality of life and require additional therapy.
Side effects:
anemia;
bloating;
chronic diarrhea;
nausea;
abdominal cramps;
nausea;
partial obstruction of the small intestine.
Methods of diagnosis

The disease is usually diagnosed based on symptoms, medical history, and results of a physical examination. At the first stage, the attending physician prescribes tests to find out the cause of enteritis. For example, a stool test in a laboratory is done to determine the type of infection. If additional diagnostics are required to clarify the information, an x-ray of the small intestine or other studies are prescribed. Analysis of tissue samples allows you to learn more about what happens in the small intestine.
Main researches:
coprogram;
PCR screening;
survey radiography;
fibrogastroduodenoscopy;
research on helminth eggs;
general blood analysis;
bacteriological culture;
Ultrasound of the abdominal organs;
video capsule endoscopy, etc.
Depending on the localization of the inflammatory process during the development of the disease, duodenitis is additionally diagnosed – a lesion of the duodenum, ileitis – the ileum, jejunum – the jejunum. Often, against the background of the disease, concomitant pathologies develop: damage to the stomach – gastroenteritis or colon – enterocolitis. Other disorders associated with the development of pathological processes are also possible.
Treatment of enteritis
The treatment plan depends on the cause of the disease. Based on the patient’s symptoms, medical history, and test results, the doctor determines the underlying cause of inflammation in the small intestine. For example, if a patient develops a fever, this indicates an infection. Therefore, treatment may require the use of antibiotics in case of a bacterial infection or antiviral drugs, which are prescribed for a virus infection. In situations where the cause of enteritis is radiation therapy, a change in the method of treatment is recommended. This can help alleviate the patient’s condition and get rid of a number of unpleasant symptoms. Alternatively, if the course of radiation therapy has already been completed, the inflammation in the small intestine can be expected to subside in a few weeks or months.
The main goal in the treatment process is to avoid dehydration and loss of electrolytes. As a result, the patient will be advised to increase fluid intake. Alternatively, intravenous drugs may be given. The patient will also be advised to rest as much as possible to regain their strength. In general, the treatment of enteritis is aimed at alleviating the patient’s condition and eliminating symptoms. The main recommendations are proper rest and rehydration. If the cause is an infection, the immune system usually does not need support, and the body fights off the diseased bacteria unaided. With a weakened immune system and other disorders, a bacterial infection can last longer. In this case, the attending physician prescribes antibiotics. In ischemia or an autoimmune disease, treatment is additionally aimed at combating the root causes of the development of a pathological condition. In chronic enteritis, anti-inflammatory drugs may be prescribed.
Medications
The treatment plan may include probiotics, antihistamines, vitamin complexes and other pharmaceuticals, which are selected by the attending physician individually in accordance with the type and form of the disease. The treatment regimen also often includes antispasmodics, antidiarrheals, sedatives and antipyretics. Please note that self-medication is not recommended. If enteritis is suspected, especially if characteristic symptoms persist for a long time, it is necessary to make an appointment with a doctor.
Diet for enteritis

If there are problems with the assimilation of food, it is recommended to change the daily diet and give preference to bland and simple dishes. Eat small, frequent meals to prevent nausea. If you’re having trouble eating solid foods, it’s worth including lean broths on your menu, which can help keep you hydrated and give you the energy boost you need. The composition and quantity of dishes are selected depending on the state. At any stage of enteritis, it is recommended to adhere to a sparing diet. During the period of exacerbation, if there are no contraindications, hunger is practiced. The patient needs to consume at least 1,5-2 liters of fluid. A decoction of herbs, rose hips, strong tea with lemon is allowed. With enteritis, often, but not more than 3-4 days, a treatment table No. 4 is prescribed, which helps to maintain a sparing diet and alleviate diarrhea.
Key recommendations:
a decrease in the volume of portions;
fractional diet;
pureed or steamed dishes;
viscous consistency of yours, soups and side dishes;
exclusion of vegetables and foods that stimulate intestinal motility.
After reducing diarrhea and before normalizing the stool, a therapeutic diet No. 4B is prescribed, which is characterized by mashed foods. Diet No. 4B is recommended for chronic enteritis, during the period of recovery and remission.
Prevention

Infectious enteritis, which is the most common, is the easiest to prevent. With careful personal hygiene, the disease rarely develops.
Basic preventive measures:
Wash your hands with soap and water after using the toilet, in public places and before handling food.
clean kitchen utensils and surfaces that have come into contact with raw meat or other non-cooked foods;
do not eat raw fish, poorly fried meat and other similar dishes;
observe the recommended mode of storage of ready meals and foodstuffs;
When traveling to foreign countries, use clean bottled water.
When traveling, carry hand sanitizer or sanitary napkins with a high alcohol content of at least 6%.
Smoking cessation and limiting alcohol consumption are also essential to prevent inflammation of the small intestine.
When should i see a doctor?
nausea lasts more than 2 days;
diarrhea for more than 24 hours;
vomiting for more than 2 days;
there are signs of dehydration;
temperature above 38°C;
blood clots in vomit or stools;
severe pain in the abdomen.
If you suspect enteritis, you should make an appointment with a general practitioner or gastroenterologist. The treatment plan and inpatient department, if hospitalization is required, are determined by the type of enteritis and the nature of the course of the disease.
[Video] VoiceGen – causes, symptoms and treatment of enteritis:









