Contents
Discectomie
The most commonly performed intervention in spinal surgery, discectomy consists of removing a herniated disc. While this is the standard surgical treatment for a herniated disc, discectomy is not, however, its first-line treatment. It is only offered in cases of very debilitating pain and after failure of drug treatments.
What is a discectomy?
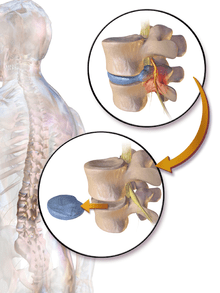
The discectomy consists of removing a herniated disc to free the nerve root stuck by the hernia, and thus make the pain associated with this compression disappear.
As a reminder, the spine is made up of vertebrae stacked on top of each other and separated by intervertebral discs. The spine is crossed at its center by the spinal canal, which contains the spinal cord. On each floor, a spinal nerve detaches from the spinal cord on either side of the intervertebral discs.
Composed of a gelatinous central nucleus and a fibrous peripheral ring, the discs act as “shock absorbers” between each vertebra. But over the years or due to daily micro-trauma or trauma, small tears or cracks may appear in the fibrous core. In the event of cracking, the nucleus can migrate into the ring, cross it and end up making a projection which will compress the nerve inside the spine: this is the herniated disc. It is diagnosed by CT and / or MRI.
If it concerns the cervical spine, the 7 vertebrae which schematically form the neck, we speak of cervical disc herniation. This can, by compression of the nerve root, cause cervicobrachial neuralgia (NCB) manifested by pain radiating from the arm to the fingers, sometimes accompanied by tingling or tingling (paresthesias), or disturbances of the tenderness (dysesthesia).
If it affects one of the discs located between the 5 vertebrae of the lumbar spine, it is called a lumbar disc herniation. This can cause pain in the leg on the side of the hernia, behind or on the side of the leg if the sciatic nerve is compressed, on the front of the thigh and the tibia if it is the crural nerve.
Depending on the location of the herniated disc, we will therefore distinguish:
- cervical discectomy;
- lumbar discectomy.
How is the discectomy?
The operation is performed under general anesthesia.
For a herniated cervical disc, the surgeon usually goes through the anterolateral route, that is to say through the front of the neck, in order to access the front of the disc. He then proceeds to the complete ablation of the disc, then to the ablation of the herniated disc, most often under microchirugie. To remedy the instability due to the removal of the disc, the surgeon can perform arthrodesis, that is to say the fusion of the two vertebrae, or else put in place a prosthesis.
For lumbar discectomy, the patient is placed in genuflection thanks to a special Z-shaped chair. The classic method consists of making an incision of about 5 cm in the affected vertebra, to detach the muscle from the vertebra, to remove the hernia and sometimes a small piece of disc. The minimally invasive technique, more and more used, reproduces the same gestures (with the difference that the muscle is not really detached from the column, but simply spread), with smaller incisions (1 to 3 cm) , under a surgical microscope (microdiscectomy) or an endoscope (microdiscectomy under endoscopy). Sometimes arthrodesis is necessary.
When to perform a discectomy?
Discectomy is not the first-line treatment for a herniated disc, whether lumbar or cervical. It is only offered in the presence of disabling pain for the patient, and after failure of prolonged treatment (4 to 8 weeks minimum) with rest, anti-inflammatory drugs, relaxants, and analgesics, or even corticosteroid infiltration. And of course, after having taken into account the benefits / risks balance of the intervention.
However, certain situations may require an emergency discectomy:
- cervicobrachial neuralgia or hyperalgesic sciatica (intolerable pain not relieved by morphine);
- paralyzing cervicobrachial neuralgia with motor deficit;
- cervicobrachial neuralgia with signs of compression of the spinal cord;
- a lumbar disc herniation leading to paralysis of the urinary and anal sphincter muscles (cauda equina syndrome);
- severe paralyzing sciatica affecting major muscles in the foot, knee or hip.
After the discectomy
Operative suites
Hospitalization lasts from 1 to a few days depending on the case.
Depending on the nature of the professional activity, the location of the hernia, the severity and duration of the symptoms, the duration of the sick leave will be from 3 to 12 weeks.
Walking is recommended as soon as you get home. It is possible to resume a sporting activity after rehabilitation and a period of 3 to 6 months depending on the type of sport and the speed of recovery.
The results
Discectomy eliminates cervicobrachial neuralgia in about 90% of cases, but has little effect on neck pain. Motor and / or sensory disorders may also persist if the nerve root has been damaged too much by the hernia.
Lumbar discectomy largely eliminates or alleviates sciatic or crural pain in 80 to 90% of cases, but its effect is less on back pain. As with a herniated cervical disc, the nerve may have been damaged or compressed for too long. Pain will then persist despite the operation. Finally, a recurrence of the hernia can occur in 5 to 10% of cases, sometimes only a few days after the operation.
The risks
In addition to the risks inherent in any surgical intervention (risks associated with general anesthesia, risk of infection of the surgical site, risk of phlebitis), discectomy is a delicate procedure because it affects the spine. It therefore involves various risks:
- the formation of a hematoma which, if large, can compress the organs of the neck and interfere with swallowing and breathing in cervical discectomy, or lead to cauda equina syndrome in lumbar discectomy. An emergency re-intervention is then necessary;
- if the spinal nerve has been affected, sensory or motor disturbances may appear. They are most often transient but sequelae are possible;
- the risk of paralysis is rare, but not zero. Neurological complications in the spinal cord can lead to quadriplegia (paralysis of the 4 limbs) for cervical discectomy, paralysis of the lower limbs for lumbar discectomy;
- displacement of the arthrodesis material, requiring reoperation;
- dysphonia (pathway disorder), generally due to irritation of the vocal cord nerve during cervical discectomy, transient but may in some cases require speech therapy;
- dysphagia (difficulty swallowing), also usually transient;
- Claude Bernard Horner syndrome, due to damage to small nerves in the neck, manifested by dryness of the face and sagging eyelid.