Contents
What is a curettage?
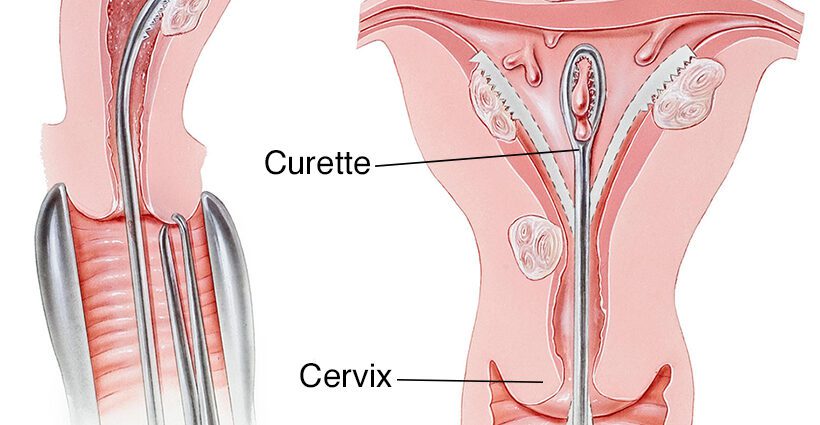
In the medical field, curettage refers to the surgical act which consists in removing (using an instrument resembling a spoon, generally called a “curette”) all or part of an organ from a natural cavity. This term is generally used in connection with the uterus. Curettage then consists of removing the tissue that covers the internal cavity of the uterus, or endometrium.
When should uterine curettage be done?
Curettage can be performed for diagnostic purposes, for example to perform an endometrial biopsy, but also, and above all, for therapeutic purposes, to eliminate endometrial residues that would not have been evacuated naturally. This is particularly the case when a spontaneous or induced miscarriage has not allowed the complete expulsion of the embryo (or the fetus), the evacuation of the placenta and the endometrium. Same thing in the context of voluntary termination of pregnancy (abortion) drug or aspiration.
By extension, the term curettage is used to refer to the suction technique, which is less invasive, less painful and less risky for the woman than a “classic” curettage. We sometimes even talk about suction curettage.
Why perform uterine curettage?
If a curettage is necessary to remove residues of the placenta or endometrium, it is because these tissues can eventually lead to complications, such asbleeding, infection, or infertility. It is therefore better to remove them carefully, after leaving a little time for a possible natural expulsion, or with the help of medication. The ideal is obviously that the expulsion takes place spontaneously and without medication, within a reasonable time to avoid any risk of infection.
How does a curettage work? Who does it?
Curettage of the uterus is performed in the operating room, under local or general anesthesia. It is conducted by a gynecological surgeon, who can sometimes administer a product to dilate the cervix before the operation in order to be able to access the uterine cavity more easily. Short, the intervention is carried out most often on an outpatient basis, with an outing the same day. Analgesics are usually prescribed to alleviate the pain that may occur in the days that follow.
What precautions after curettage?
When there has been a miscarriage or abortion, the cervix has opened. Just as it can take several hours or days to open, the cervix can take a long time to close. When the cervix is open, the uterus can be exposed to germs, which can lead to infection. As after pregnancy, it is recommended after a curettage ofavoid baths, swimming pool, sauna, hammam, tampons, menstrual cups and sexual intercourse for a fortnight at least, to limit the risks.
Otherwise, if severe pain, fever or heavy bleeding occurs a few days after a curettage, it is better to inform your gynecologist. He will then carry out another check-up to check if all the residues are gone, to make sure there are no signs of infection, etc.
Curettage: what are the risks and complications for a new pregnancy?
Curettage performed with a “curette” is an invasive procedure which, like any procedure in the uterus, can create adhesions in the uterine cavity. It then happens, in rare cases, that these injuries and adhesions make it difficult for a new pregnancy to occur, or that they hinder the evacuation of the rules. We call Asherman’s syndrome, or uterine synechia, a uterine disease characterized by the presence of adhesions in the uterus, and which may occur following poorly conducted curettage. The diagnosis of synechia must be made before:
- irregular cycles,
- less heavy periods (or even an absence of periods),
- the presence of cyclic pelvic pain,
- infertility.
A hysteroscopy, that is to say an endoscopic examination of the uterine cavity, can then be performed to determine or not the presence of post-curettage or post-aspiration adhesions, and choose the treatment accordingly.
Note that the aspiration technique, which is currently often preferred to surgery, represents less risk.
How long to leave before a pregnancy after a curettage?
Once we have ensured via an ultrasound that no residue of uterine lining (or endometrium) or placenta has escaped curettage, and that the uterine cavity is therefore healthy, in theory nothing opposes upon the onset of a new pregnancy. If ovulation occurs in the cycle following miscarriage or abortion, pregnancy may well occur.
Medically, it is believed today, with some exceptions, that there is no contraindication to trying to get pregnant after curettage, just like after a spontaneous miscarriage without intervention.
In practice, it is for each woman and each couple to know if they feel ready to try again to carry out a pregnancy. Physically, bleeding and period pain-like pain may occur in the days following curettage. And psychologically, it may be important to take the time. Because a miscarriage or an abortion can be experienced as difficult ordeals. When the pregnancy was desired, put words on this loss, recognize the existence of a little being whose arrival we wished and say goodbye … Grieving is important. For an abortion, the psychological aspect is also fundamental. Abortion or miscarriage, each woman and each couple experiences this event in their own way. The important thing is to surround yourself well, to accept your sadness, in order to set off again on a good basis, and possibly, to consider a new pregnancy with as much serenity as possible.
Medically, pregnancy after a well-performed curettage does not present no more risk than a typical pregnancy. There is no no more risk of miscarriage after curettage. Done properly, curettage does not render infertile or otherwise sterile.