Contents
Cow’s milk intolerance in infants: what to do?
Cow’s milk protein allergy, or APLV, is the most common food allergy in infants. It most often appears in the first months of life. As these symptoms vary greatly from one child to another, its diagnosis can sometimes be difficult. Once the diagnosis is made, APLV requires an elimination diet, under medical supervision. Allergy with a good prognosis, it naturally evolves towards the development of tolerance in the majority of children.
Cow’s milk allergy: what is it?
The composition du lait de vache
Cow’s milk protein allergy, or APLV, refers to the occurrence of clinical manifestations after ingestion of cow’s milk or dairy products, following an abnormal immunological reaction against cow’s milk proteins. Cow’s milk contains around thirty different proteins, with among others:
- lactalbumin,
- β-lactoglobulin,
- bovine serum albumin,
- bovine immunoglobulins,
- caséines αs1, αs2, β et al.
They are potential allergens. PLVs are one of the main allergens in the first 2 years of life, which makes sense since in the first year, milk is the baby’s main food.
The different pathologies
Depending on the mechanism involved, there are different pathologies:
IgE dependent cow’s milk allergy (IgE-mediated)
or the APLV itself. The proteins in cow’s milk induce an inflammatory response with the production of immunoglobulin E (IgE), antibodies produced in response to an allergen.
Non-IgE dependent milk intolerance
The body reacts with different symptoms to exposure to cow’s milk antigens, but there is no production of IgE. In infants, this is the most common form.
APLV can affect a baby’s growth and bone mineralization because nutrients are not absorbed well.
How do you know if your baby is APLV?
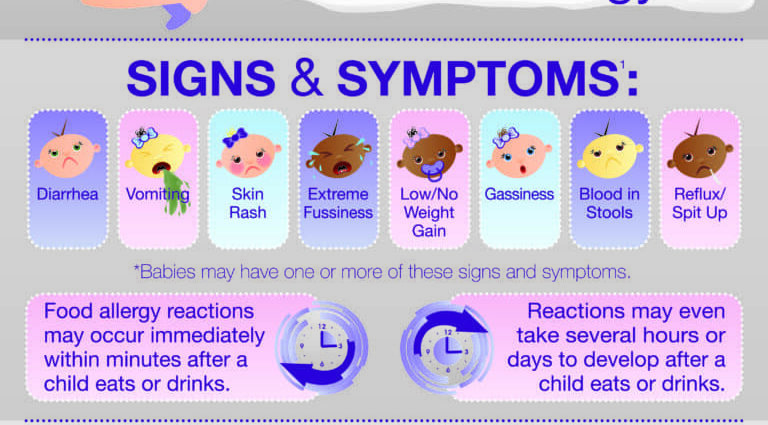
The clinical manifestations of APLV are highly variable depending on the underlying mechanism, the child and his age. They affect both the digestive system, the skin, the respiratory system.
In case of IgE-mediated APLV
In IgE-mediated APLV, reactions are usually immediate: oral syndrome and vomiting followed by diarrhea, generalized reactions with pruritus, urticaria, angioedema, and in more severe cases anaphylaxis.
In case of unmediated IgE
In case of unmediated IgE, manifestations are usually delayed:
- eczema (atopic dermatitis);
- diarrhea or, on the contrary, constipation;
- persistent regurgitation or even vomiting;
- des rectorragies;
- colic, abdominal pain;
- bloating and gas;
- insufficient weight gain;
- irritability, sleep disturbances;
- rhinitis, chronic cough;
- frequent ear infections;
- infant asthma.
These manifestations are very different from one baby to another. The same child can have both immediate and delayed reactions. Symptoms also change with age: before 1 years of age, skin and digestive symptoms are more common. Afterwards, the APLV manifests itself more by cutaneous-mucous and respiratory signs. These are all factors that sometimes make the diagnosis of APLV difficult.
How to diagnose APLV in the baby?
Faced with digestive and / or skin signs in the baby, the doctor will first of all carry out a clinical examination and an interrogation on the various allergic reactions, the baby’s diet, his behavior or even the family history of allergy. In particular, the doctor can use the CoMiSS® (Cow’s milk-related symptom score), a score based on the main symptoms related to APLV.
The different tests to diagnose an APLV
Today, there are no biological tests that can establish or refute with certainty a diagnosis of APLV. The diagnosis is therefore based on various tests.
For IgE-dependent APLV
- a cow’s milk skin prick test. This skin test involves making a small amount of purified allergen extract penetrate the skin with a small lancet. 10 to 20 minutes later, the result is obtained. A positive test is manifested by a papule, (a small pimple). This test can be done very early on in infants, and is completely painless.
- a blood test for specific IgE.
For a non-IgE dependent APLV
- a patch test or patch test. Small cups containing the allergen are placed on the skin of the back. They are removed 48 hours later, and the result is obtained 24 hours later. The positive reactions range from a simple simple erythema to a combination of erythema, vesicles and bubbles.
The diagnosis with certainty is made by an eviction test (the cow’s milk proteins are eliminated from the diet) and by oral challenge to cow’s milk proteins, regardless of the immunological form.
What alternative to milk for an APLV baby?
The management of APLV is based on strict elimination of the allergen. Specific milks will be prescribed to the baby, according to the recommendations of the Nutrition Committee of the French Pediatric Society (CNSFP) and the European Society for Pediatric Gastroenterology Hepatology and Nutrition (ESPGHAN).
The use of an extensive protein hydrolyzate (EO)
In first intention, an extensive hydrolyzate of proteins (EO) or high hydrolyzate of proteins (HPP) will be offered to the baby. These milks prepared from casein or whey are in the majority of cases well tolerated by APLV infants. If the symptoms persist after having tested the different types of hydrolysates, or in the event of severe allergic symptoms, an infant formula based on synthetic amino acids (FAA) will be prescribed.
Soy milk protein preparations
Soymilk protein (PPS) preparations are generally well tolerated, cheaper and taste better than hydrolysates, but their isoflavone content is questionable. These phytochemicals present in soy are phytoestrogens: due to their molecular similarities, they can mimic estrogens, and therefore act as endocrine disruptors. They are prescribed as a third line, preferably after 6 months, making sure to choose a milk with a reduced isoflavone content.
Hypoallergenic milk (HA)
Hypoallergenic (HA) milk is not indicated in the case of APLV. This milk, made from cow’s milk, which has been modified to make it less allergenic, is intended for prevention for babies with allergies (notably family history), on medical advice, during the baby’s first six months.
The use of vegetable juices
The use of vegetable juices (soy, rice, almond and others) is strongly discouraged, as they are not adapted to the nutritional needs of infants. As for the milk of other animals (mare, goat), they do not provide all the nutrients necessary for the baby either, and may cause other allergic reactions, due to the risk of cross-allergies.
How is the reintroduction of POS?
The elimination diet should last for at least 6 months or until the age of 9 or even 12 or 18 months, depending on the severity of the symptoms. The gradual reintroduction will take place after an oral challenge test (OPT) with cow’s milk performed in the hospital.
APLV has a good prognosis thanks to the progressive maturation of the intestinal immune system of the child and the acquisition of tolerance to milk proteins. In the majority of cases, the natural course is towards the development of tolerance in children between 1 and 3 years of age: approximately 50% by the age of 1 year,> 75% by the age of 3 years and> 90% at the age of 6.
APLV and breastfeeding
In breastfed babies, the incidence of APLV is very low (0,5%). The management of APLV in a breastfed baby consists of eliminating all dairy products from the mother’s diet: milk, yogurt, cheese, butter, sour cream, etc. At the same time, the mother must take vitamin D and calcium supplementation. If the symptoms improve or disappear, the nursing mother can try the gradual reintroduction of cow’s milk proteins into her diet, without exceeding the maximum dose tolerated by the child.