Cholesteatoma: definition and review of this infection
Cholesteatoma consists of a mass made up of epidermal cells, located behind the tympanic membrane, which gradually invades the structures of the middle ear, gradually damaging them. Cholesteatoma most often follows a chronic infection that has gone unnoticed. If not treated in time, it can destroy the middle ear and lead to deafness, infection, or facial paralysis. It can also spread to the inner ear and cause dizziness, even to brain structures (meningitis, abscess). The diagnosis is based on the demonstration of a whitish mass in the external auditory canal. The rock scan completes the assessment by highlighting the extension of this mass within the structures of the ear. Cholesteatoma requires rapid treatment. This is completely removed during surgery, passing through the back of the ear. A second surgical intervention may be indicated to ensure the absence of recurrence and to reconstruct the ossicles at a distance.
What is a cholesteatoma?
Cholesteatoma was first described in 1683 under the name of “ear decay” by Joseph Duverney, the father of otology, the branch of medicine specializing in the diagnosis and treatment of disorders. of the human ear.
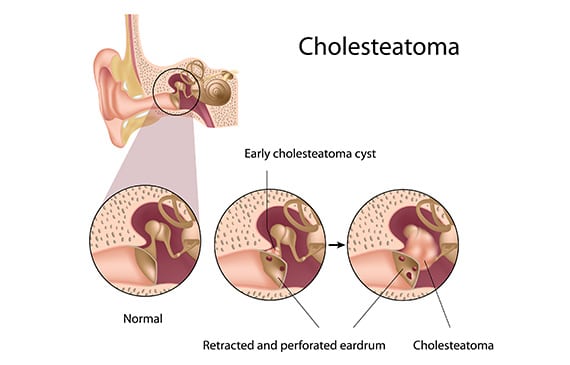
Cholesteatoma is defined by the presence of epidermis, i.e. skin, inside the cavities of the middle ear, in the eardrum, behind the tympanic membrane and / or in the mastoid, areas normally devoid of skin.
This buildup of skin, which looks like a cyst or a pocket filled with skin scales, will gradually grow in size leading to chronic middle ear infection and destruction of surrounding bone structures. Therefore, cholesteatoma is called dangerous chronic otitis.
There are two types of cholesteatoma:
- acquired cholesteatoma: this is the most common form. It forms from a retraction pocket of the tympanic membrane, which will gradually invade the mastoid and the middle ear, destroying the structures in contact with it;
- congenital cholesteatoma: this represents 2 to 4% of cholesteatoma cases. It comes from an embryological remnant of skin in the middle ear. This rest will gradually produce new skin debris which will accumulate in the middle ear, often in the anterior part, and first produce a small mass of whitish appearance, behind the tympanic membrane which has remained intact, most often in children or young adults, without particular symptoms. If not detected, this mass will gradually grow and behave like an acquired cholesteatoma, causing hearing loss and then other symptoms depending on the damage produced in the ear. When cholesteatoma causes discharge, it has already reached an advanced stage.
What are the causes of cholesteatoma?
Cholesteatoma most often follows recurrent ear infections due to a malfunction of the eustachian tube responsible for a tympanic retraction pocket. In this case, the cholesteatoma corresponds to the culmination of the evolution of an unstable retraction pocket.
Other less common causes of cholesteatoma exist such as:
- traumatic perforation of the eardrum;
- ear trauma such as a rock fracture;
- ear surgery such as tympanoplasty or otosclerosis surgery.
Finally, more rarely, in the case of congenital cholesteatoma, it can be present from birth.
What are the symptoms of cholesteatoma?
Cholesteatoma is responsible for:
- sensation of blocked ear;
- recurrent unilateral otitis in adults or children;
- Repeated unilateral otorrhea, that is, chronic purulent ear discharge, yellowish in color and foul-smelling (smell of “old cheese”), not calmed by medical treatment or prevention strict aquatic;
- earache, which is pain in the ear;
- otorrhagia, that is, bleeding from the ear;
- inflammatory polyps of the eardrum;
- progressive reduction in hearing: whether it appears at the beginning or whether it is of variable evolution, hearing impairment often concerns only one ear, but can be bilateral. This deafness first presents itself in the form of serous otitis. It can worsen as a result of the slow bone destruction of the chain of ossicles in contact with the retraction pocket which develops into a cholesteatoma. Finally, in the long term, the growth of the cholesteatoma can destroy the inner ear and therefore be responsible for complete deafness or cophosis;
- facial paralysis: infrequent, it corresponds to the suffering of the facial nerve in contact with the cholesteatoma;
- feeling of dizziness and balance disorders: infrequent, they are linked to the opening of the inner ear by the cholesteatoma;
- rare serious infections such as mastoiditis, meningitis, or brain abscess, following the development of cholesteatoma in the temporal brain region near the ear.
How to detect a cholesteatoma?
The diagnosis of cholesteatoma is based on:
- otoscopy, that is to say the clinical examination, carried out using a microscope by the specialist ENT specialist, which makes it possible to diagnose a discharge from the ear, an otitis, a retraction pocket, or a skin cyst, the only clinical aspect confirming the presence of cholesteatoma;
- an audiogram, or hearing measurement. At the onset of the disease, hearing impairment is mainly located in the middle ear. It is therefore classically detected a pure conductive hearing loss linked to the modification of the tympanic membrane or the progressive destruction of the chain of ossicles in the middle ear. The bone conduction curve that tests the inner ear is then strictly normal. Gradually, over time and the growth of the cholesteatoma, there may appear a decrease in bone conduction responsible for so-called “mixed” deafness (sensorineural hearing loss associated with conductive hearing loss) and highly in favor of the onset of destruction. of the inner ear requiring treatment without delay;
- a rock scan: it must be systematically requested for surgical management. By visualizing an opacity with convex edges in the compartments of the middle ear with the presence of bone destruction on contact, this radiological examination makes it possible to confirm the diagnosis of cholesteatoma, to specify its extension and to look for possible complications;
- an MRI may be requested especially in case of doubt about a recurrence after treatment.
How to treat a cholesteatoma?
When the diagnosis of cholesteatoma is confirmed, the only possible treatment is its removal by surgery.
Objectives of the intervention
The aim of the intervention is to perform the total ablation of the cholesteatoma, while preserving or improving hearing, balance and facial function if its location in the middle ear allows it. The requirements related to the removal of cholesteatoma can sometimes explain the impossibility of preserving or improving hearing, or even the deterioration of hearing after the operation.
Several types of surgical interventions can be performed:
- tympanoplasty in closed technique;
- tympanoplasty in open technique;
- petro-mastoid recess.
The choice between these different techniques is decided and discussed with the ENT surgeon. It depends on several factors:
- extension of cholesteatoma;
- state of hearing;
- anatomical conformation;
- desire to resume aquatic activities;
- possibilities of medical surveillance;
- operative risk etc.
Carrying out the intervention
This is performed under general anesthesia, retro-auricular, that is to say through the back of the ear, during a short hospital stay of a few days. The facial nerve is monitored continuously throughout the operation. The intervention consists, after extraction of the cholesteatoma sent for anatomo-pathological examination, to leave as little residue as possible and to reconstruct the eardrum via cartilage taken from the tragal region, that is to say at the front of the auditory canal. external, or at the back of the concha of the auricle.
Convalescence and post-operative follow-up
In case of chain of ossicles damaged by cholesteatoma, if the ear is not too infected, reconstruction of the hearing is done during this first surgical intervention by replacing the destroyed ossicle with a prosthesis.
Clinical and radiological monitoring (CT scan and MRI) must be done regularly because of the high potential for recurrence of cholesteatoma. It is necessary to see the patient again 6 months after the operation and to systematically schedule an imaging examination at 1 year. In the event of no restoration of hearing, doubtful radiological image or in favor of recurrence, abnormal otoscopy or deterioration of hearing despite satisfactory reconstruction of the latter, a second surgical intervention is required. to plan 9 to 18 months after the first, in order to check the absence of residual cholesteatoma and to try to improve the hearing.
In the event that there is no second intervention to be planned, an annual clinical monitoring is carried out over several years. Definitive cure is considered in the absence of recurrence more than 5 years after the last surgical intervention.