Contents
Autoimmune disease: definition, causes and treatments
An autoimmune disease is the result of an anomaly in the immune system leading the latter to attack the normal components of the organism (the “self”, hence the root auto- to speak of this immunity disorder) . A classic distinction is made between organ-specific autoimmune diseases, which affect a particular organ (such as autoimmune diseases of the thyroid), and systemic autoimmune diseases, such as lupus, which can affect several organs.
Understanding these diseases
While it is supposed to protect us from pathogens (which can cause disease), our immune system can sometimes go out of order. It can then become too sensitive to certain exogenous (external) constituents, and trigger allergies or react against constituents of the self and promote the emergence of autoimmune diseases.
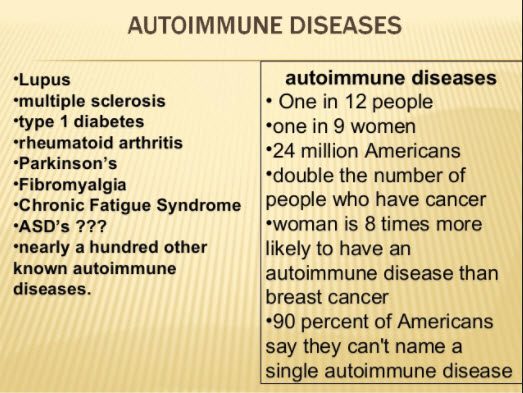
Autoimmune diseases form a group in which we find diseases as different as type I diabetes, multiple sclerosis, thumatoid arthritis or Crohn’s disease. They all correspond to chronic diseases triggered by the organism’s loss of immunological tolerance to its own constituents.
How are autoimmune diseases established?
A true internal army made up of several white blood cells, the immune system defends the body against external attacks such as bacteria or viruses and usually tolerates its own constituents. When self-tolerance breaks down, it becomes a source of disease. Some white blood cells (autoreactive lymphocytes) specifically attack tissues or organs.
Antibodies normally produced by certain immune cells to neutralize the enemy by attaching to certain molecules (antigens) can also appear and target elements of our body. The body secretes antibodies against its own antigens which it considers foreign.
For example:
- in type I diabetes: autoantibodies target insulin-secreting pancreatic cells;
- in rheumatoid arthritis: it is the membrane that surrounds the joints that is targeted, the inflammation spreads to the cartilages, bones, even tendons and ligaments;
- in systemic lupus erythematosus, auto-anticoprs are directed against molecules present in many cells of the body, leading to damage to several organs (skin, joints, kidneys, heart, etc.).
In some cases, we do not find autoantibodies and we speak rather of “autoinflammatory” diseases. The body’s first line of defense immune cells (neutrophils, macrophages, monocytes, natural killer cells) alone trigger chronic inflammation leading to the destruction of certain tissues:
- skin in psoriasis (which affects 3 to 5% of the European population);
- certain joints in rheumatoid spondylitis;
- the digestive tract in Crohn’s disease;
- the central nervous system in multiple sclerosis.
Whether they are strictly autoimmune or auto-inflammatory, all of these diseases result from a dysfunction of the immune system and develop into chronic inflammatory diseases.
Who is concerned ?
At the start of the 5st century, autoimmune diseases affect around 80 million people in France and have become the third cause of mortality / morbidity after cancer and cardiovascular diseases and in roughly the same proportions. XNUMX% of cases concern women. Today, if treatments make it possible to slow down their development, autoimmune diseases remain incurable.
The causes of autoimmune diseases
The vast majority of autoimmune diseases are multifactorial. With a few exceptions, they are considered to be based on the combination of genetic, endogenous, exogenous and / or environmental, hormonal, infectious and psychological factors.
The genetic background is important, hence the often familial nature of these diseases. For example, the frequency of type I diabetes goes from 0,4% in the general population to 5% in relatives of a diabetic.
In ankylosing spondylitis, the HLA-B27 gene is present in 80% of affected subjects but in only 7% of healthy subjects. Dozens if not hundreds of genes have been associated with each autoimmune disease.
Experimental studies or epidemiological data clearly describe an association between the intestinal microbiota (digestive ecosystem), which is located at the interface between the immune system and the environment, and the occurrence of an autoimmune disease. There are exchanges, a kind of dialogue, between the intestinal bacteria and the immune cells.
The environment (exposure to microbes, certain chemicals, UV rays, smoking, stress, etc.) also plays a major role.
Diagnostic
The search for an autoimmune disease must always be done in an evocative context. Examinations include:
- exploration to diagnose affected organs (clinical, biological, organ biopsy);
- a blood test to search for inflammation (non-specific) but which can point to the severity of the attacks and to explore the immunological assessment with a search for autoantibodies;
- systematic search for possible complications (kidney, lungs, heart and nervous system).
What treatment for autoimmune diseases?
Each autoimmune disease responds to specific treatment.
Treatments make it possible to control the symptoms of the disease: analgesics against pain, anti-inflammatory drugs against functional discomfort in the joints, replacement drugs making it possible to normalize endocrine disorders (insulin for diabetes, thyroxine in hyothyroidism).
Drugs that control or inhibit autoimmunity also offer a way to limit symptoms and the progression of tissue damage. They usually have to be taken chronically because they cannot cure the disease. In addition, they are not specific to autoimmunity effector cells and interfere with certain general functions of the immune system.
Historically, immunosuppressive drugs (corticosteroids, cyclophosphamide, methotrexate, ciclosporin) have been used because they interact with central effectors of the immune system and make it possible to limit its activity overall. They are often associated with an increased risk of infection and therefore require regular monitoring.
For twenty years, biotherapies have been developed: they offer better control of symptoms. These are molecules that specifically target one of the key players involved in the process concerned. These treatments are used when the disease is severe or does not respond or sufficiently to immunosuppressants.
In the case of very specific pathologies such as Guillain Barre syndrome, plasmapheresis allows the elimination of autoantibodies by filtration of the blood which is then reinjected into the patient.